AI and the Future of Cardiovascular Treatments
In recent years, artificial intelligence (AI) has emerged as a game changer in the medical field, particularly in the realm of cardiovascular care. Imagine a world where doctors can predict heart problems before they even occur, or where treatment plans are tailored specifically to your unique genetic makeup. This is not science fiction; it’s the reality we are stepping into. The integration of AI in cardiovascular treatments is not just enhancing diagnosis and treatment; it’s fundamentally transforming how healthcare is delivered. As we delve deeper into this topic, we’ll explore the various ways AI is enhancing cardiovascular care, the ethical considerations it raises, and what the future holds for both healthcare professionals and patients alike.
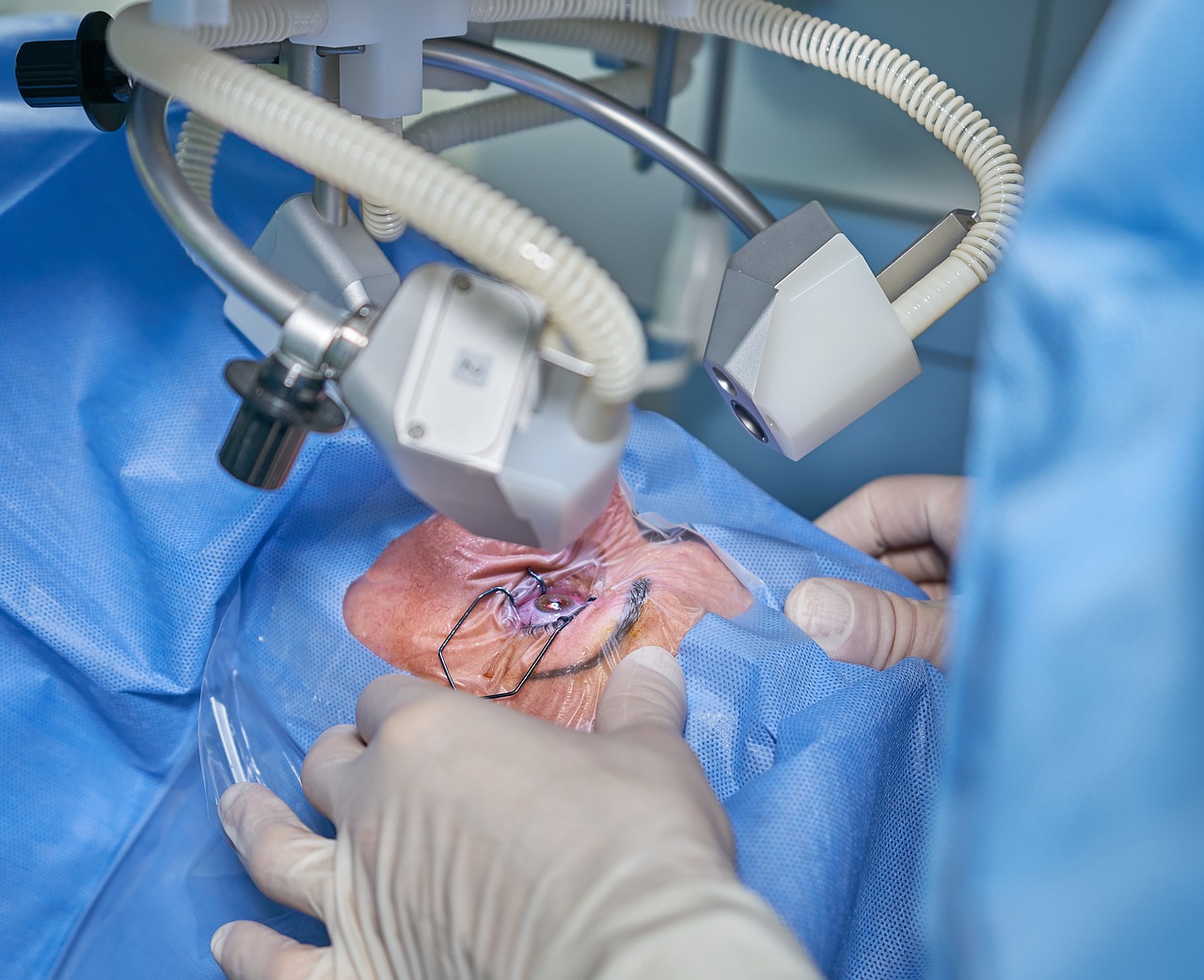
AI technologies are revolutionizing the diagnostic processes in cardiology, enabling faster and more accurate identification of cardiovascular diseases through advanced imaging and data analysis techniques. Traditional diagnostic methods often rely heavily on human interpretation, which can lead to errors or delays. However, with AI, we can analyze complex imaging data at lightning speed. For instance, AI algorithms can process thousands of echocardiograms in the time it takes a human to review just a handful. This not only reduces the waiting time for patients but also increases the likelihood of early detection, which is crucial for effective treatment.
Predictive analytics powered by AI can forecast patient outcomes, allowing healthcare providers to tailor treatments and interventions based on individual risk factors and historical data. Imagine being able to predict a heart attack years in advance based on your lifestyle, genetic factors, and medical history. This level of foresight enables doctors to implement preventive measures that can save lives. For example, if a patient shows signs of high cholesterol and has a family history of heart disease, AI can flag this risk and prompt the healthcare provider to initiate early interventions.
Machine learning algorithms analyze vast datasets to identify patterns that help predict cardiovascular events, enhancing preventive care strategies and improving patient management. These algorithms are constantly learning and evolving, making them incredibly powerful tools in the fight against heart disease. They can sift through data from electronic health records, wearable devices, and even social determinants of health to create a comprehensive risk profile for each patient.
Various data sources, including electronic health records and wearable devices, contribute to the efficacy of machine learning algorithms in predicting cardiovascular risks. For instance, data from smartwatches that monitor heart rates and physical activity can provide real-time insights into a patient’s cardiovascular health. This information can be invaluable for healthcare providers as they develop personalized treatment plans.
Despite the potential benefits, challenges such as data privacy, algorithm transparency, and integration into existing workflows hinder the widespread adoption of machine learning in cardiovascular care. Patients often worry about how their data will be used and protected. Moreover, healthcare providers need to ensure that these algorithms are reliable and free from biases that could affect patient outcomes.
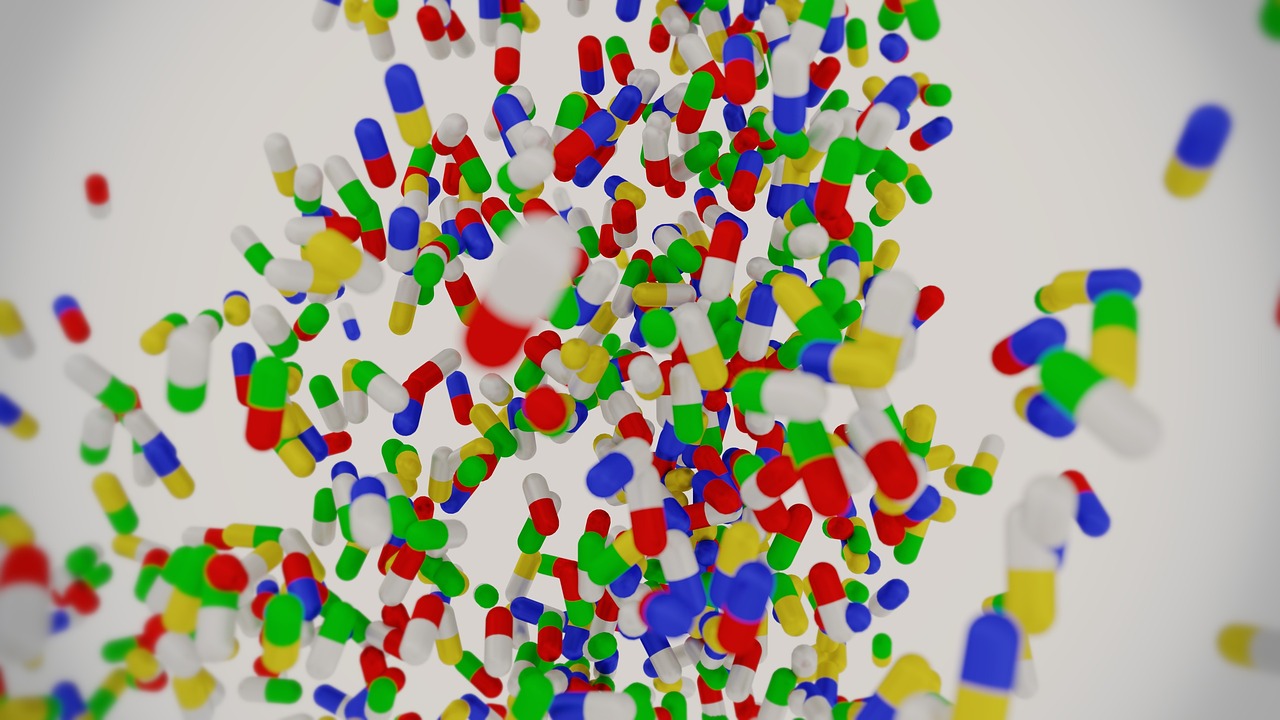
AI assists in creating personalized treatment plans by analyzing patient data and recommending tailored therapies, thus improving adherence and outcomes for cardiovascular patients. By considering a patient's unique characteristics, AI can suggest the most effective medications, lifestyle changes, and follow-up schedules. This level of personalization can significantly enhance patient engagement and improve overall health outcomes.
AI enhances remote monitoring capabilities, allowing healthcare providers to track patient progress and adjust treatment plans in real-time, thus improving access to care and patient engagement. With the rise of telemedicine, patients can receive high-quality care without having to leave their homes. This is especially beneficial for those in rural or underserved areas where access to specialized care may be limited.
Wearable devices equipped with AI capabilities enable continuous monitoring of cardiovascular metrics, providing valuable insights for both patients and healthcare providers. These devices can alert users to irregular heartbeats, sudden changes in blood pressure, or other concerning metrics. This real-time feedback empowers patients to take charge of their health and make informed decisions.
Telehealth platforms utilizing AI facilitate virtual consultations, making cardiovascular care more accessible, especially for patients in remote or underserved areas. These innovations not only save time and resources but also ensure that patients receive timely interventions, which can be crucial in managing cardiovascular diseases.
The integration of AI in cardiovascular treatments raises ethical questions regarding data privacy, bias in algorithms, and the role of healthcare professionals in decision-making processes. As we embrace these technologies, it’s vital to address these concerns to maintain trust between patients and providers.
Efforts must be made to identify and mitigate biases in AI algorithms to ensure equitable treatment outcomes across diverse patient populations in cardiovascular care. If the data used to train these algorithms is not representative of the general population, certain groups may be unfairly disadvantaged. Thus, ongoing evaluation and adjustment of these systems are necessary.
Ensuring informed patient consent and protecting privacy are crucial as AI technologies collect and analyze sensitive health data in cardiovascular treatments. Patients should be fully aware of how their data will be used and have the right to opt-out if they choose. Transparency is key in fostering a trusting relationship between patients and healthcare providers.
The future of AI in cardiology promises advancements in personalized medicine, enhanced patient engagement, and improved healthcare delivery, transforming how cardiovascular diseases are managed and treated. As technology continues to evolve, we can expect even more innovative solutions that will reshape the landscape of cardiovascular care.
Integrating AI with genomic data could lead to breakthroughs in understanding the genetic factors influencing cardiovascular diseases, paving the way for targeted therapies. By analyzing genetic markers alongside traditional risk factors, healthcare providers can develop even more precise treatment strategies.
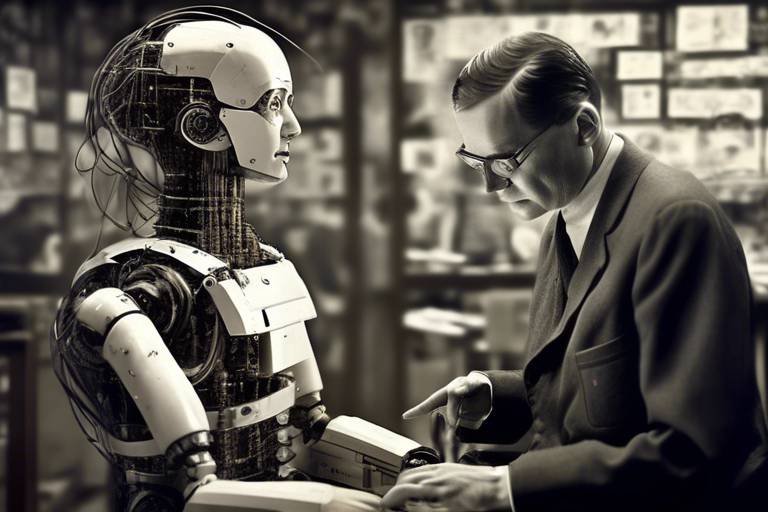
The partnership between AI technologies and healthcare professionals will be essential in harnessing the full potential of AI for improved cardiovascular outcomes. While AI can provide valuable insights and recommendations, the human touch remains irreplaceable. Doctors will play a crucial role in interpreting AI findings and making informed decisions based on their clinical expertise.
- What is AI's role in cardiovascular diagnosis? AI enhances diagnostic accuracy and speed through advanced imaging and data analysis.
- How can predictive analytics improve patient outcomes? By forecasting risks and tailoring treatments to individual patients, predictive analytics can lead to better health outcomes.
- What are some challenges in implementing AI in healthcare? Data privacy, algorithm bias, and integration with existing healthcare workflows are significant challenges.
- How does telemedicine benefit cardiovascular care? Telemedicine increases access to care and allows for real-time monitoring and adjustments to treatment plans.

The Role of AI in Diagnosis
Artificial Intelligence (AI) is making waves in the realm of cardiology, particularly in the diagnostic processes. Imagine a world where heart diseases can be detected earlier and with greater accuracy than ever before. That’s the promise AI brings to the table! With the power of advanced imaging and data analysis techniques, AI is transforming how healthcare professionals identify cardiovascular diseases. This transformation is not just a mere upgrade; it’s akin to switching from a horse-drawn carriage to a high-speed train!
One of the standout features of AI in diagnosis is its ability to analyze vast amounts of data at lightning speed. Traditional methods often rely on human interpretation, which can be subjective and prone to error. However, AI algorithms can sift through complex datasets, identifying patterns that might escape even the most experienced cardiologists. For example, AI can analyze echocardiograms, MRIs, and CT scans with a level of precision that significantly reduces the chances of misdiagnosis.
Furthermore, AI doesn’t just stop at identifying existing conditions. It also plays a crucial role in predictive diagnostics. By evaluating historical data and current patient metrics, AI can forecast potential heart issues before they become critical. This proactive approach is a game-changer, allowing for timely interventions that can save lives. Imagine being able to predict a heart attack days or even weeks in advance; that’s the kind of future AI is helping to create.
To give you a clearer picture, let’s look at some of the key technologies that are driving AI in cardiovascular diagnosis:
| Technology | Description | Benefits |
|---|---|---|
| Deep Learning | A subset of machine learning that uses neural networks to analyze images. | Improves accuracy in image interpretation. |
| Natural Language Processing (NLP) | AI that understands and processes human language. | Enhances the extraction of relevant information from patient records. |
| Predictive Analytics | Analyzes historical patient data to predict future health events. | Allows for personalized preventive care strategies. |
As we dive deeper into the role of AI in diagnosis, it’s essential to recognize the challenges it faces. While the technology is impressive, it’s not without its hurdles. Issues such as data privacy, the need for robust datasets, and the integration of AI tools into existing healthcare systems can complicate its implementation. However, the potential benefits far outweigh these challenges, making the investment in AI technologies a worthwhile endeavor for the future of cardiovascular care.
In conclusion, AI is not just a passing trend in cardiology; it’s a revolutionary force that is reshaping how we diagnose heart diseases. With its ability to provide faster, more accurate diagnoses and predictive insights, AI is paving the way for a new era of cardiovascular care. It empowers healthcare professionals to make informed decisions and ultimately enhances patient outcomes, making it an exciting time to be involved in this field.

Predictive Analytics for Patient Outcomes
Predictive analytics is paving the way for a new era in cardiovascular care, where data-driven insights lead to better patient outcomes. Imagine having the ability to foresee potential health issues before they even arise; that's the magic of predictive analytics powered by artificial intelligence (AI). By leveraging vast amounts of data, healthcare providers can make informed decisions tailored to individual patients, significantly enhancing the quality of care.
At its core, predictive analytics involves the use of statistical algorithms and machine learning techniques to identify the likelihood of future outcomes based on historical data. In the realm of cardiology, this means analyzing everything from patient demographics to lifestyle choices and medical history. For instance, by examining patterns in electronic health records, AI can highlight patients at high risk for heart attacks or strokes, allowing for timely interventions. The beauty of this approach lies in its ability to turn data into actionable insights, ultimately leading to personalized treatment plans that cater to the unique needs of each patient.
One of the standout features of predictive analytics is its ability to incorporate real-time data. This means that as new information becomes available—be it from a recent doctor's visit or changes in a patient's health metrics—AI systems can adjust predictions and recommendations accordingly. This dynamic adaptability ensures that healthcare providers are always equipped with the most current information, fostering a proactive rather than reactive approach to patient care.
Moreover, predictive analytics can also enhance patient engagement. When patients are informed about their risks and the rationale behind their treatment plans, they are more likely to adhere to prescribed therapies. This not only improves health outcomes but also empowers patients, making them active participants in their own healthcare journeys. To illustrate this, consider a scenario where a patient receives a notification from their healthcare provider about an increased risk of cardiovascular events based on their latest health data. This timely alert allows the patient to make lifestyle changes or seek further medical advice, ultimately leading to better management of their condition.
However, it's essential to acknowledge that the implementation of predictive analytics is not without challenges. Data privacy concerns loom large, as sensitive health information is being processed and analyzed. Healthcare organizations must ensure robust security measures are in place to protect patient data while still reaping the benefits of these advanced analytics. Additionally, there is a need for transparency in how algorithms make predictions, as understanding the "why" behind a recommendation can foster trust between patients and healthcare providers.
In summary, predictive analytics is revolutionizing how we approach cardiovascular care. By harnessing the power of AI, healthcare providers can anticipate patient needs, tailor treatment plans, and ultimately improve outcomes. As we continue to navigate this exciting landscape, the collaboration between technology and healthcare professionals will be crucial in ensuring that predictive analytics is used ethically and effectively.
- What is predictive analytics in healthcare?
Predictive analytics in healthcare involves using statistical algorithms and machine learning techniques to analyze historical data and predict future health outcomes. - How does predictive analytics improve patient outcomes?
By identifying patients at risk of cardiovascular events and personalizing treatment plans, predictive analytics enables proactive care, improving overall health outcomes. - What are the challenges of implementing predictive analytics?
Key challenges include data privacy concerns, the need for transparency in algorithms, and the integration of predictive tools into existing healthcare workflows.

Machine Learning Algorithms
Machine learning algorithms are at the forefront of revolutionizing how we approach cardiovascular care. They sift through massive amounts of data, identifying patterns that the human eye might miss. Imagine a detective examining thousands of clues to solve a case—this is how machine learning operates, but instead of clues, it analyzes health metrics, patient histories, and diagnostic images. By leveraging these algorithms, healthcare professionals can enhance their predictive capabilities, leading to earlier interventions and better patient outcomes.
One of the most exciting aspects of machine learning in cardiology is its ability to predict cardiovascular events before they occur. For instance, algorithms can analyze a patient’s electronic health records (EHRs) and lifestyle factors to assess their risk of developing heart disease. This predictive power allows doctors to intervene proactively, potentially saving lives. The algorithms continuously learn and improve over time, adapting to new data, which means the predictions become more accurate as more information is fed into the system.
To illustrate the impact of machine learning, consider the following table that summarizes some key applications:
| Application | Description | Benefits |
|---|---|---|
| Risk Assessment | Evaluates patient data to determine the likelihood of cardiovascular events. | Early intervention and personalized care. |
| Image Analysis | Analyzes echocardiograms and MRIs for abnormalities. | Faster and more accurate diagnoses. |
| Treatment Optimization | Suggests personalized treatment plans based on patient history. | Improved adherence and outcomes. |
However, the implementation of machine learning algorithms is not without its challenges. For instance, the quality of predictions is heavily dependent on the data used to train the algorithms. If the data is biased or incomplete, the results can lead to misdiagnoses or inappropriate treatment plans. Furthermore, integrating these advanced technologies into existing healthcare workflows requires significant investment in training and infrastructure. It’s essential for healthcare providers to ensure that these tools complement human expertise rather than replace it.
In conclusion, machine learning algorithms hold immense potential in transforming cardiovascular care. By harnessing the power of data, they enable healthcare professionals to make informed decisions that can significantly improve patient outcomes. As we continue to explore this exciting frontier, the collaboration between technology and human insight will be crucial in navigating the complexities of cardiovascular treatment.
- What are machine learning algorithms?
Machine learning algorithms are computational methods that analyze large datasets to identify patterns and make predictions based on the data. - How do these algorithms improve cardiovascular care?
They enhance risk assessment, improve diagnostic accuracy, and personalize treatment plans, leading to better patient outcomes. - What challenges exist in implementing machine learning in healthcare?
Challenges include data quality, algorithm bias, and the need for integration into existing healthcare systems. - Can machine learning replace healthcare professionals?
No, machine learning is designed to assist healthcare professionals, providing them with valuable insights to enhance their decision-making process.

Data Sources for Machine Learning
In the realm of cardiovascular care, the effectiveness of machine learning algorithms heavily relies on the quality and diversity of data sources. These algorithms thrive on vast amounts of information, which they analyze to identify patterns and make predictions about patient outcomes. The primary data sources utilized in this context include electronic health records (EHRs), wearable devices, and clinical studies.
Electronic health records serve as a treasure trove of patient information, encompassing medical history, treatment plans, and outcomes. By harnessing EHRs, machine learning models can uncover trends that may not be visible through traditional analysis. For instance, they can pinpoint which treatment protocols yield the best results for specific patient demographics, thereby enhancing personalized care.
Wearable devices, such as smartwatches and fitness trackers, have become increasingly popular in monitoring cardiovascular health. These devices provide real-time data on vital signs like heart rate, blood pressure, and physical activity levels. The continuous stream of information generated by wearables offers a unique opportunity for machine learning algorithms to detect anomalies and predict potential cardiovascular events before they escalate into serious health issues.
Moreover, clinical studies contribute significantly to the data pool, offering insights into the efficacy of various treatments and interventions. By analyzing data from diverse clinical trials, machine learning can help identify which therapies work best for different patient profiles, thus paving the way for more targeted treatment plans.
However, the integration of these data sources into machine learning frameworks is not without its challenges. For instance, data quality can vary significantly, and inconsistent data formats can complicate analysis. Additionally, ensuring the privacy and security of sensitive health information is paramount, as breaches could undermine patient trust and violate regulations.
In summary, the synergy between machine learning and data sources such as EHRs, wearable technology, and clinical studies is crucial for advancing cardiovascular care. As we continue to refine these data inputs, the potential for improved patient outcomes becomes even more promising.
- What are electronic health records (EHRs)? EHRs are digital versions of patients' paper charts, containing comprehensive medical histories, treatment plans, and test results.
- How do wearable devices contribute to cardiovascular care? Wearable devices monitor vital health metrics in real-time, providing continuous data that can help predict and manage cardiovascular conditions.
- What are the main challenges in using data for machine learning? Challenges include data quality, privacy concerns, and the need for standardization across different data sources.

Challenges in Implementation
Implementing AI in cardiovascular care is akin to navigating a complex maze. While the potential benefits are immense, several challenges stand in the way of seamless integration. First and foremost, data privacy concerns loom large. As AI systems require access to vast amounts of sensitive patient data, ensuring that this information is protected from breaches is critical. Healthcare providers must comply with stringent regulations, such as HIPAA in the United States, which adds layers of complexity to the implementation process.
Another significant hurdle is algorithm transparency. Many AI algorithms operate as "black boxes," making it difficult for healthcare professionals to understand how decisions are made. This lack of transparency can lead to mistrust among practitioners and patients alike. If a doctor cannot explain why a specific treatment is recommended, it raises ethical questions about accountability and patient safety.
Moreover, integrating AI into existing workflows presents its own set of challenges. Healthcare systems are often burdened with legacy technologies that are not designed to accommodate advanced AI solutions. This can lead to inefficiencies and frustration among healthcare providers who are trying to deliver the best care possible. Training staff to effectively use these new tools is also essential, as a lack of familiarity can hinder the adoption of AI technologies.
To summarize, the challenges in implementing AI in cardiovascular care can be categorized as follows:
- Data Privacy: Protecting sensitive patient information is paramount.
- Algorithm Transparency: Understanding how AI makes decisions is crucial for trust.
- Integration with Existing Workflows: Legacy systems can complicate the adoption of new technologies.
- Staff Training: Ensuring that healthcare providers are well-versed in AI tools is vital for successful implementation.
Addressing these challenges requires a collaborative effort between technology developers, healthcare providers, and regulatory bodies. Only through open dialogue and innovative solutions can we hope to unlock the full potential of AI in transforming cardiovascular care.
- What are the main challenges in implementing AI in cardiovascular care?
Data privacy, algorithm transparency, integration with existing systems, and staff training are some of the key challenges. - How does AI improve cardiovascular diagnosis?
AI enhances diagnostic accuracy by analyzing complex data sets and identifying patterns that may be missed by human practitioners. - What role does data privacy play in AI implementation?
Data privacy is crucial as AI systems need access to sensitive patient information, and protecting this data is essential for compliance and trust. - Can AI replace healthcare professionals in cardiovascular care?
No, AI is designed to assist healthcare professionals by providing insights and recommendations, not to replace their expertise.

AI-Driven Treatment Plans
In the rapidly evolving landscape of healthcare, are becoming a game-changer for patients suffering from cardiovascular diseases. Imagine walking into a clinic where your treatment is not just a one-size-fits-all approach but is tailored specifically to your unique health profile. This is no longer a distant dream; it’s a reality being shaped by artificial intelligence. By analyzing vast amounts of data, AI can suggest personalized therapies that take into account not just the disease but also the individual’s lifestyle, genetics, and even preferences.
AI systems leverage machine learning algorithms to sift through extensive patient records, clinical studies, and real-time health data. This allows healthcare providers to create treatment plans that are not only effective but also enhance patient adherence. For instance, if a patient has a history of poor compliance with medication, AI can recommend a regimen that includes easier-to-take medications or alternative therapies that fit better into the patient’s daily routine. This level of personalization leads to better outcomes and fosters a sense of trust between patients and their healthcare providers.
Moreover, AI can continuously learn and adapt treatment plans based on ongoing patient data. If a patient’s condition changes or if they experience side effects, AI can suggest modifications in real-time. This dynamic approach is akin to having a personal health coach who is always in tune with your needs, making adjustments as necessary. It’s not just about treating a condition; it’s about managing health holistically.
However, the implementation of AI-driven treatment plans is not without challenges. Data privacy is a significant concern; sensitive health information must be protected while still allowing AI systems to analyze it effectively. Additionally, there’s the question of algorithm transparency. Patients and healthcare providers alike need to understand how AI arrives at its recommendations to foster trust and ensure ethical practices.
In summary, AI-driven treatment plans represent a significant leap forward in cardiovascular care. They promise not only improved health outcomes but also a more engaged patient experience. As we continue to integrate these technologies into clinical practice, the future of cardiovascular treatment looks brighter than ever.
- What is an AI-driven treatment plan?
AI-driven treatment plans are personalized healthcare strategies created using artificial intelligence to analyze patient data, ensuring that treatments are tailored to individual needs. - How does AI improve patient adherence to treatment?
By suggesting personalized therapies that fit better into a patient's lifestyle and preferences, AI enhances the likelihood that patients will follow their treatment plans. - What are the challenges of implementing AI in treatment plans?
Challenges include data privacy concerns and the need for transparency in how AI algorithms make decisions. - Can AI adapt treatment plans over time?
Yes, AI can continuously learn from ongoing patient data and suggest modifications to treatment plans as needed.

Remote Monitoring and Telemedicine
In today's fast-paced world, remote monitoring and telemedicine are reshaping the landscape of cardiovascular care. Imagine being able to receive high-quality medical attention without ever stepping foot in a hospital. Sounds incredible, right? Well, thanks to advancements in technology, this is becoming a reality for many patients. Remote monitoring allows healthcare providers to keep a close eye on patients' health metrics in real-time, while telemedicine facilitates virtual consultations, bridging the gap between patients and doctors regardless of geographical barriers.
One of the most exciting aspects of remote monitoring is the use of wearable technology. Devices like smartwatches and fitness trackers can continuously monitor vital signs such as heart rate, blood pressure, and even oxygen levels. This constant stream of data not only helps patients stay informed about their health but also empowers healthcare providers to make timely interventions. For instance, if a patient's heart rate spikes unexpectedly, an alert can be sent to their doctor, prompting immediate action. This level of proactive care is a game-changer in managing cardiovascular diseases.
Moreover, telemedicine has made it easier for patients in remote or underserved areas to access specialized care. With just a few clicks, patients can schedule virtual appointments with cardiologists, eliminating the need for long travel times and reducing the burden on healthcare facilities. This is especially beneficial for elderly patients or those with mobility issues who may find it challenging to visit a clinic in person. Telehealth platforms equipped with AI can even assist in triaging patients, ensuring that those who need urgent care are prioritized.
However, while these innovations are undeniably beneficial, they also come with their own set of challenges. For example, not all patients are tech-savvy, and some may struggle to use the necessary devices or applications. Additionally, there are concerns about data security and privacy, as sensitive health information is transmitted over the internet. It's crucial for healthcare providers to ensure that robust security measures are in place to protect patient data.
As we move forward, the integration of remote monitoring and telemedicine into cardiovascular care will likely become even more seamless. Imagine a future where AI algorithms analyze data from wearable devices, alerting healthcare providers about potential issues before they escalate. This could lead to a more personalized approach to treatment, where interventions are tailored to each patient's unique needs. The combination of technology and human expertise could revolutionize how we manage cardiovascular health.
- What is remote monitoring in cardiovascular care?
Remote monitoring involves using technology, such as wearable devices, to track patients' health metrics in real-time, allowing healthcare providers to monitor their condition without in-person visits. - How does telemedicine work for cardiovascular patients?
Telemedicine allows patients to consult with healthcare providers via video calls or online platforms, making it easier to access care from the comfort of their homes. - What are the benefits of using wearable technology?
Wearable devices can continuously monitor vital signs, provide alerts for any concerning changes, and empower patients to take charge of their health. - Are there any risks associated with remote monitoring and telemedicine?
While these technologies offer numerous benefits, they also pose challenges such as data privacy concerns and the need for patients to be comfortable using technology.

Wearable Technology
Wearable technology has taken the healthcare world by storm, especially in the realm of cardiovascular care. Imagine having a personal health assistant strapped to your wrist or tucked into your pocket, constantly monitoring your heart rate, blood pressure, and even your stress levels. Sounds futuristic, right? But that’s exactly what these devices offer! With the integration of artificial intelligence, wearables are not just passive monitors; they actively analyze data and provide real-time feedback to both patients and healthcare providers.
These devices, which range from smartwatches to specialized health monitors, are equipped with sensors that track a variety of cardiovascular metrics. For instance, a smartwatch can monitor your heart rate continuously, alerting you if it detects any irregularities that might indicate a potential issue. This capability is crucial because early detection can lead to timely interventions, ultimately saving lives. The data collected can be transmitted directly to healthcare providers, allowing for proactive management of cardiovascular health.
Moreover, the insights gained from wearable technology can empower patients to take charge of their health. When individuals can see their heart rate trends or receive notifications about their activity levels, they are more likely to engage in healthier behaviors. For example, a patient might receive a prompt to take a walk after sitting for too long, or reminders to take medication at the right time. This kind of engagement not only enhances adherence to treatment plans but also fosters a sense of responsibility towards one’s health.
However, while wearables offer exciting possibilities, they also come with challenges. One major concern is the accuracy of the data collected. Not all wearable devices are created equal; some may provide misleading information, leading to unnecessary anxiety or, conversely, complacency. It's essential for consumers to choose reputable brands and for healthcare providers to understand the limitations of these devices. Furthermore, as with any technology that collects personal health data, privacy is a significant concern. Patients must be assured that their data is handled securely and ethically.
In summary, wearable technology represents a significant leap forward in cardiovascular care. By providing real-time monitoring, enhancing patient engagement, and facilitating proactive healthcare management, these devices have the potential to transform how we approach heart health. As technology continues to evolve, we can expect even greater innovations that will further integrate AI into wearables, making them smarter and more effective in managing cardiovascular diseases.
- What types of wearable devices are best for monitoring cardiovascular health?
Devices like smartwatches and fitness trackers from reputable brands such as Apple, Fitbit, and Garmin are popular choices. They typically offer heart rate monitoring, activity tracking, and even ECG capabilities.
- Can wearable technology replace regular check-ups with healthcare providers?
While wearables can provide valuable data, they should complement, not replace, regular medical check-ups. Always consult with healthcare professionals for comprehensive care.
- How secure is the personal health data collected by wearables?
Data security varies by device and manufacturer. It's crucial to choose devices that prioritize data privacy and comply with regulations like HIPAA.
- Are wearables suitable for everyone?
While many people can benefit from wearables, those with specific health conditions should consult their healthcare provider to determine the best approach for monitoring their health.

Telehealth Innovations
In recent years, have emerged as a game-changer in the field of cardiovascular care. Imagine being able to consult with your cardiologist from the comfort of your own home, without the hassle of waiting rooms and long drives. This is no longer just a dream; it’s becoming a reality thanks to advancements in technology. Telehealth platforms are now equipped with artificial intelligence (AI) capabilities that enhance the quality of remote consultations, making cardiovascular care more accessible than ever.
One of the most significant benefits of telehealth is its ability to bridge the gap between patients and healthcare providers, especially for those living in remote or underserved areas. Patients can now receive timely consultations, follow-up appointments, and even emergency care without needing to travel long distances. This is particularly crucial for individuals with chronic cardiovascular conditions who require consistent monitoring and support. By utilizing telehealth, healthcare providers can ensure that patients stay engaged in their treatment plans while also reducing the burden on healthcare facilities.
Moreover, telehealth innovations have made it possible for healthcare providers to leverage real-time data from wearable devices. These devices can monitor vital signs, such as heart rate and blood pressure, and transmit this information directly to healthcare professionals. This continuous flow of data allows for proactive interventions and timely adjustments to treatment plans, ultimately leading to better patient outcomes. For instance, if a patient's heart rate spikes, the healthcare provider can quickly assess the situation and provide immediate guidance or treatment recommendations.
As we look to the future, the integration of AI in telehealth is expected to evolve further. For example, AI algorithms can analyze patient data to identify trends and predict potential health issues before they escalate. This predictive capability is particularly beneficial in cardiovascular care, where early intervention can be lifesaving. By analyzing data patterns, AI can help healthcare providers determine which patients may be at higher risk for heart attacks or other cardiovascular events, allowing for timely and targeted interventions.
In addition to improving access and monitoring, telehealth innovations also enhance the overall patient experience. Virtual consultations can be more convenient and comfortable for patients, reducing the anxiety often associated with in-person visits. With the ability to consult from home, patients are more likely to adhere to their follow-up appointments and treatment plans. This increase in engagement is crucial for managing cardiovascular diseases effectively.
However, while the benefits of telehealth are clear, there are still challenges to address. Issues such as technology access, internet connectivity, and patient comfort with digital tools can impact the effectiveness of telehealth solutions. It’s essential for healthcare providers to offer support and education to help patients navigate these platforms. As we continue to innovate in telehealth, addressing these challenges will be key to maximizing its potential in cardiovascular care.
- What is telehealth? Telehealth refers to the use of technology to provide healthcare services remotely, allowing patients to consult with healthcare providers via video calls, phone calls, or messaging.
- How does telehealth benefit cardiovascular patients? Telehealth improves access to care, enables real-time monitoring of health metrics, and allows for timely interventions, thus enhancing patient engagement and outcomes.
- Are telehealth consultations secure? Yes, most telehealth platforms prioritize patient privacy and use encrypted communication methods to protect sensitive health information.
- Can telehealth replace in-person visits? While telehealth can significantly enhance care, it may not fully replace in-person visits, especially for procedures that require physical examinations or tests.
Ethical Considerations in AI Use
The integration of artificial intelligence in cardiovascular treatments is not just a technological advancement; it also brings forth a plethora of ethical considerations that must be addressed to ensure fair and effective healthcare delivery. As we race towards a future where AI plays a pivotal role in patient care, we must pause and reflect on the implications of its use. One of the primary concerns revolves around data privacy. With AI systems processing vast amounts of sensitive health information, the risk of data breaches becomes a significant issue. Patients must feel confident that their personal data is protected, and that there are stringent measures in place to prevent unauthorized access.
Another major ethical dilemma is the potential for algorithmic bias. AI systems learn from historical data, which can inadvertently include biases present in that data. For instance, if a machine learning model is trained predominantly on data from one demographic group, it may not perform as well for others, leading to disparities in treatment outcomes. This bias can exacerbate existing health inequalities, making it crucial for developers and healthcare providers to actively seek ways to identify and mitigate such biases.
Furthermore, the role of healthcare professionals in the decision-making process raises important questions. As AI systems become more sophisticated, there is a risk that healthcare providers may overly rely on these technologies, potentially undermining their clinical judgment. It's vital to strike a balance where AI serves as a supportive tool rather than a replacement for human expertise. This leads us to the need for informed patient consent. Patients should be fully aware of how AI technologies will be used in their care, and they must consent to the collection and analysis of their health data. This transparency is essential in fostering trust between patients and healthcare providers.
In light of these considerations, healthcare institutions must implement comprehensive frameworks to address these ethical challenges. This includes establishing guidelines for the responsible use of AI, ensuring that patient rights are upheld, and fostering a culture of accountability. By doing so, we can harness the power of AI in cardiovascular treatments while safeguarding the integrity of patient care.
- What are the main ethical concerns regarding AI in healthcare?
The primary concerns include data privacy, algorithmic bias, and the role of healthcare professionals in decision-making.
- How can algorithmic bias be addressed?
By actively identifying biases in training data and ensuring diverse datasets are used, developers can mitigate the risks of bias in AI algorithms.
- Why is informed patient consent important?
Informed consent ensures that patients understand how their data will be used and helps build trust in the healthcare system.

Addressing Algorithmic Bias
In the rapidly evolving landscape of AI in cardiovascular care, one of the most pressing issues is algorithmic bias. This bias occurs when AI systems produce systematically prejudiced results due to erroneous assumptions in the machine learning process. Imagine a scenario where a predictive model misidentifies a high-risk patient simply because the data it was trained on lacked diversity. Such a situation not only undermines the effectiveness of AI tools but also poses significant risks to patient care and outcomes.
To effectively address algorithmic bias, it is crucial to implement a multi-faceted approach that includes:
- Diverse Data Collection: Gathering data from a wide range of populations is essential. This means including various demographics such as age, gender, ethnicity, and socioeconomic status to ensure that the algorithms can learn from a representative sample.
- Regular Audits: Continuous monitoring and auditing of AI systems can help identify biases that may emerge over time. This process should involve healthcare professionals who can provide insights into the clinical relevance of the data.
- Transparent Algorithms: Developing transparent algorithms that allow for scrutiny and understanding of how decisions are made is vital. This transparency builds trust among healthcare providers and patients alike.
Moreover, collaboration between AI developers and healthcare professionals is key. By working together, they can ensure that the algorithms are not only technically sound but also clinically applicable. For instance, a team of cardiologists and data scientists can review the datasets used for training AI models to identify potential biases and correct them before they impact patient care.
Ultimately, addressing algorithmic bias is not just a technical challenge; it’s a moral imperative. By ensuring that AI tools are equitable and effective for all patients, we can enhance the overall quality of cardiovascular care. As we move forward, it is essential to foster an environment where ethical considerations are at the forefront of AI development, ensuring that technology serves to bridge gaps in healthcare rather than widen them.
- What is algorithmic bias? Algorithmic bias refers to systematic and unfair discrimination that occurs when an AI system produces prejudiced results due to flawed data or assumptions in the model.
- How can we mitigate algorithmic bias in healthcare? Mitigation strategies include diverse data collection, regular audits of AI systems, and promoting transparency in algorithm development.
- Why is addressing algorithmic bias important? Addressing algorithmic bias is crucial to ensure equitable treatment outcomes, improve patient safety, and enhance the overall effectiveness of AI in healthcare.
Patient Consent and Privacy
In the rapidly evolving landscape of artificial intelligence (AI) in cardiovascular treatments, the importance of patient consent and privacy cannot be overstated. As AI technologies become more integrated into healthcare, they often require access to sensitive patient data, which raises significant ethical and legal questions. It's crucial for healthcare providers to ensure that patients are fully informed about how their data will be used, stored, and shared. This transparency fosters trust, which is essential for effective treatment and patient engagement.
One key aspect of patient consent is ensuring that individuals understand the implications of AI-driven decisions in their care. For instance, when algorithms analyze data to recommend treatment plans, patients should be aware of how these recommendations are generated and the potential risks involved. In an era where data breaches are becoming alarmingly common, patients deserve to know that their information is being handled with the utmost care and security.
To address these concerns, healthcare organizations must implement robust policies that prioritize patient privacy. This includes adopting advanced cybersecurity measures to protect data and regularly updating protocols to comply with legal standards such as the Health Insurance Portability and Accountability Act (HIPAA). Moreover, organizations should provide patients with clear and concise information about their rights regarding data usage, allowing them to make informed decisions about their healthcare.
Another consideration is the role of informed consent in AI applications. Patients should have the option to opt-in or opt-out of AI-driven analyses, ensuring that they maintain control over their health information. This could involve a simple consent form that outlines how AI will be utilized in their treatment, what data will be collected, and the potential benefits and risks. By empowering patients to make choices about their care, healthcare providers can enhance the therapeutic relationship and encourage greater participation in their health journeys.
Furthermore, as AI systems are trained on diverse datasets, it's vital to address the issue of algorithmic bias that could affect patient outcomes. If certain demographics are underrepresented in training data, AI algorithms may produce skewed results, leading to disparities in care. In this context, patient consent also involves ensuring that algorithms are developed and tested with a diverse population in mind, promoting equitable healthcare for all.
In conclusion, prioritizing patient consent and privacy is essential as AI continues to reshape cardiovascular treatments. By fostering transparency, ensuring informed consent, and addressing algorithmic bias, healthcare providers can navigate the complexities of AI integration while upholding the rights and dignity of their patients.
- What is patient consent in the context of AI?
Patient consent refers to the process of informing patients about how their data will be used in AI applications and obtaining their permission to use that data for analysis and treatment recommendations. - How does AI impact patient privacy?
AI can enhance patient privacy by implementing advanced security measures to protect sensitive health information. However, it also raises concerns about data breaches and unauthorized access, making it essential for healthcare providers to prioritize data protection. - What can patients do to ensure their privacy?
Patients should ask healthcare providers about their data protection policies, understand how their information will be used, and have the option to opt-out of AI analyses if they feel uncomfortable. - How can healthcare organizations address algorithmic bias?
Healthcare organizations can address algorithmic bias by ensuring that AI systems are trained on diverse datasets and regularly auditing algorithms for fairness and equity in treatment recommendations.

Future Trends in AI and Cardiology
The future of AI in cardiology is not just promising; it’s downright exciting! As we look ahead, we can expect a wave of innovations that will fundamentally change how cardiovascular diseases are managed and treated. One of the most significant trends is the move towards personalized medicine. Imagine a world where treatments are tailored specifically to your genetic makeup and lifestyle. This isn’t science fiction; it’s the future we’re heading towards, thanks to the integration of AI with genomic data.
By analyzing genetic information alongside traditional health data, AI can help identify the unique risk factors that contribute to cardiovascular diseases in individuals. This means that doctors could prescribe targeted therapies that are more effective and have fewer side effects. Think of it as customizing a suit; it fits better and looks sharper than something off the rack!
Moreover, we will see enhanced patient engagement as AI technologies become more user-friendly and accessible. Imagine a scenario where your smartwatch not only tracks your heart rate but also communicates directly with your healthcare provider. This kind of real-time data exchange empowers patients to take charge of their health and fosters a collaborative relationship with their doctors. It’s like having a personal trainer and nutritionist right on your wrist, guiding you towards better health!
As we embrace these advancements, the collaboration between AI and healthcare professionals will be crucial. It’s not about replacing doctors; rather, it’s about augmenting their capabilities. AI can handle the heavy lifting of data analysis, allowing healthcare providers to focus on what they do best: caring for patients. This partnership will lead to improved cardiovascular outcomes, as clinicians can make more informed decisions based on comprehensive data insights.
However, as we dive deeper into the world of AI and cardiology, we must also be mindful of the challenges that lie ahead. Issues such as data privacy, algorithmic bias, and the need for transparency in AI decision-making processes will be at the forefront of discussions. As we integrate these technologies into everyday practice, we must ensure that ethical considerations are not an afterthought but a foundational aspect of AI development.
In summary, the future of AI in cardiology is a thrilling journey filled with potential. From personalized treatment plans to enhanced patient engagement and ethical considerations, the landscape is evolving rapidly. As we move forward, we must embrace these changes while remaining vigilant about the challenges they present. The heart of the matter is that AI has the potential to revolutionize cardiovascular care, making it more effective, efficient, and equitable for all.
- What is personalized medicine in cardiology? Personalized medicine refers to tailoring medical treatment to the individual characteristics of each patient, often using genetic information to guide therapy choices.
- How does AI improve patient engagement? AI enhances patient engagement by providing real-time health data and insights, enabling patients to actively participate in their care.
- What are the ethical concerns with AI in healthcare? Ethical concerns include data privacy, potential biases in algorithms, and the need for transparency in AI-driven decision-making.
- Will AI replace doctors in cardiology? No, AI is designed to assist healthcare professionals, not replace them. It helps analyze data and provides insights, allowing doctors to focus more on patient care.

Integration with Genomics
The integration of artificial intelligence (AI) with genomics is a revolutionary step in the field of cardiology, offering unprecedented opportunities to understand the complex genetic underpinnings of cardiovascular diseases. Imagine being able to pinpoint the exact genetic variations that predispose an individual to heart disease, allowing for personalized treatment strategies that are tailored specifically to their genetic makeup. This synergy between AI and genomics not only enhances our understanding of cardiovascular conditions but also paves the way for innovative treatment approaches.
As we delve deeper into the genetic components of cardiovascular health, AI algorithms can analyze vast amounts of genomic data to identify patterns and correlations that would be impossible for human researchers to detect alone. For instance, machine learning models can sift through millions of genetic sequences, identifying specific variants associated with increased risk of conditions such as hypertension or coronary artery disease. This process can significantly accelerate the pace of research and clinical applications, transforming how we approach prevention and treatment.
One of the most exciting prospects of this integration is the potential for targeted therapies. By understanding the genetic factors at play, healthcare providers can develop treatments that target the specific pathways involved in a patient's cardiovascular disease. For example, if a patient's genomic data reveals a mutation that affects cholesterol metabolism, clinicians could prescribe medications that specifically address that metabolic pathway, leading to more effective outcomes.
Moreover, the application of AI in genomic analysis can enhance the predictive capabilities of cardiovascular care. By combining genomic information with traditional risk factors—such as age, lifestyle, and family history—AI can generate a comprehensive risk profile for each patient. This holistic view allows healthcare providers to implement preventive measures much earlier, potentially averting the onset of serious cardiovascular events.
However, the integration of AI and genomics does not come without its challenges. Issues such as data privacy and the ethical implications of genetic testing must be carefully navigated. Patients must be assured that their genetic information is handled securely and that they are fully informed about how their data will be used. Furthermore, as we harness the power of AI, it is crucial to ensure that the algorithms are free from biases that could skew results and lead to inequitable healthcare outcomes.
In conclusion, the integration of AI with genomics in cardiology represents a frontier of medical science that holds great promise. As we continue to explore this intersection, we can expect significant advancements in our ability to diagnose, treat, and ultimately prevent cardiovascular diseases. The future of heart health is not just about treating symptoms; it's about understanding the very genetic foundations of those symptoms, and AI is poised to lead the charge.
- What is the role of AI in genomics?
AI helps analyze large genomic datasets to identify patterns and correlations, enhancing our understanding of genetic factors in diseases. - How can AI improve cardiovascular treatment?
By integrating genomic data, AI can help create personalized treatment plans that target specific genetic variations associated with cardiovascular diseases. - What are the ethical concerns regarding AI and genomics?
Key concerns include data privacy, informed consent, and potential biases in AI algorithms that could affect treatment outcomes. - Will AI replace healthcare professionals in cardiology?
No, AI is intended to assist healthcare professionals by providing insights and recommendations, enhancing their decision-making capabilities.

Collaboration Between AI and Healthcare Professionals
The collaboration between artificial intelligence (AI) and healthcare professionals is not just a trend; it's a vital partnership that is reshaping the landscape of cardiovascular care. Imagine a world where doctors are equipped with AI tools that can analyze patient data faster than any human ever could, helping them make informed decisions in real-time. This synergy allows healthcare providers to focus more on patient interaction and less on administrative tasks, ultimately enhancing the quality of care.
AI can process enormous amounts of data from various sources, including electronic health records, clinical studies, and even real-time patient monitoring devices. For instance, when a cardiologist sees a patient, they can access AI-generated insights that summarize the patient’s history, risk factors, and even suggest potential treatment options. This is not just about speed; it’s about improving accuracy and reducing the likelihood of human error. The result? A more personalized and effective approach to cardiovascular treatments.
However, this collaboration isn’t without its challenges. Healthcare professionals must be trained to interpret AI-generated insights accurately and incorporate them into their clinical decision-making processes. It's essential for doctors to understand the limitations of AI, as well as its strengths. For example, while AI can identify patterns in data that may not be immediately apparent to human eyes, it cannot replace the empathetic touch that healthcare providers offer. This human element is crucial in building trust and ensuring that patients feel cared for and understood.
Moreover, the integration of AI into clinical workflows must be seamless. If healthcare professionals find AI tools cumbersome or disruptive, the potential benefits could be lost. Therefore, developers of AI technologies should work closely with healthcare practitioners to create user-friendly interfaces and functionalities that meet their needs. This collaboration can lead to innovations that not only improve patient outcomes but also enhance the overall experience for healthcare providers.
In summary, the collaboration between AI and healthcare professionals is poised to revolutionize cardiovascular care. By harnessing the strengths of both AI and human expertise, we can look forward to a future where patient care is more efficient, personalized, and effective. As we embrace this technology, it’s crucial to ensure that the human touch remains at the forefront of healthcare.
- How does AI improve cardiovascular diagnosis?
AI enhances diagnosis by analyzing medical images and patient data rapidly, allowing for quicker and more accurate identification of cardiovascular diseases. - Can AI predict patient outcomes?
Yes, AI uses predictive analytics to forecast patient outcomes based on historical data and individual risk factors, helping tailor interventions accordingly. - What role do healthcare professionals play in AI integration?
Healthcare professionals are essential for interpreting AI insights, ensuring that technology complements their expertise while maintaining patient care quality. - Are there ethical concerns with AI in healthcare?
Yes, ethical considerations include data privacy, algorithmic bias, and the need for informed patient consent as AI technologies evolve.
Frequently Asked Questions
- How is AI transforming cardiovascular diagnosis?
AI is revolutionizing cardiovascular diagnosis by enabling faster and more accurate identification of diseases through advanced imaging techniques and data analysis. This means that healthcare professionals can detect conditions much earlier, improving patient outcomes significantly.
- What role do predictive analytics play in cardiovascular care?
Predictive analytics powered by AI helps forecast patient outcomes by analyzing individual risk factors and historical data. This allows healthcare providers to tailor treatments specifically to each patient, ultimately enhancing the effectiveness of interventions.
- Can AI algorithms predict cardiovascular events?
Yes! Machine learning algorithms can analyze vast datasets to identify patterns that help predict cardiovascular events. This predictive capability enhances preventive care strategies and improves overall patient management.
- What are the challenges in implementing AI in cardiovascular care?
While AI has immense potential, challenges such as data privacy concerns, algorithm transparency, and the integration of these technologies into existing healthcare workflows can hinder widespread adoption.
- How does AI assist in creating personalized treatment plans?
AI analyzes patient data to recommend tailored therapies, which helps improve adherence to treatment and outcomes for cardiovascular patients. This personalized approach ensures that each patient receives the most effective care possible.
- What advancements does AI bring to remote monitoring and telemedicine?
AI enhances remote monitoring capabilities, allowing healthcare providers to track patient progress in real-time and adjust treatment plans as needed. This leads to better access to care and increased patient engagement, especially for those in underserved areas.
- How do wearable technologies contribute to cardiovascular health?
Wearable devices equipped with AI capabilities enable continuous monitoring of cardiovascular metrics. They provide valuable insights for both patients and healthcare providers, making it easier to manage health conditions effectively.
- What ethical considerations arise with AI in cardiovascular treatments?
The integration of AI raises important ethical questions regarding data privacy, potential biases in algorithms, and the involvement of healthcare professionals in decision-making processes. Addressing these concerns is crucial for ensuring equitable and responsible use of AI.
- How can algorithmic bias be addressed in AI systems?
Efforts must be made to identify and mitigate biases in AI algorithms to ensure fair treatment outcomes across diverse patient populations. This can involve regular audits of algorithms and incorporating diverse data sets into their training.
- What does the future hold for AI in cardiology?
The future of AI in cardiology looks promising, with advancements in personalized medicine, enhanced patient engagement, and improved healthcare delivery on the horizon. Collaborations between AI technologies and healthcare professionals will be key to unlocking these benefits.
- How might AI integrate with genomic data in the future?
Integrating AI with genomic data could lead to breakthroughs in understanding the genetic factors influencing cardiovascular diseases. This integration may pave the way for more targeted therapies, improving treatment outcomes significantly.