Impact of Nanotechnology in Medicine: A Deep Dive
Nanotechnology is not just a buzzword; it’s a revolutionary force reshaping the landscape of medicine. Imagine being able to manipulate materials at an atomic or molecular scale—this is the essence of nanotechnology. By working at the nanoscale, scientists and researchers are discovering innovative solutions that were once thought to be the stuff of science fiction. From enhancing drug delivery systems to creating advanced diagnostic tools, the impact of nanotechnology in medicine is profound and far-reaching.
At its core, nanotechnology involves the manipulation of matter at dimensions between 1 and 100 nanometers. To put that into perspective, a nanometer is one-billionth of a meter! This tiny scale opens up a world of possibilities, allowing for unprecedented control over the properties of materials. In medicine, this translates into highly effective therapies and diagnostic techniques that can target diseases more precisely than ever before.
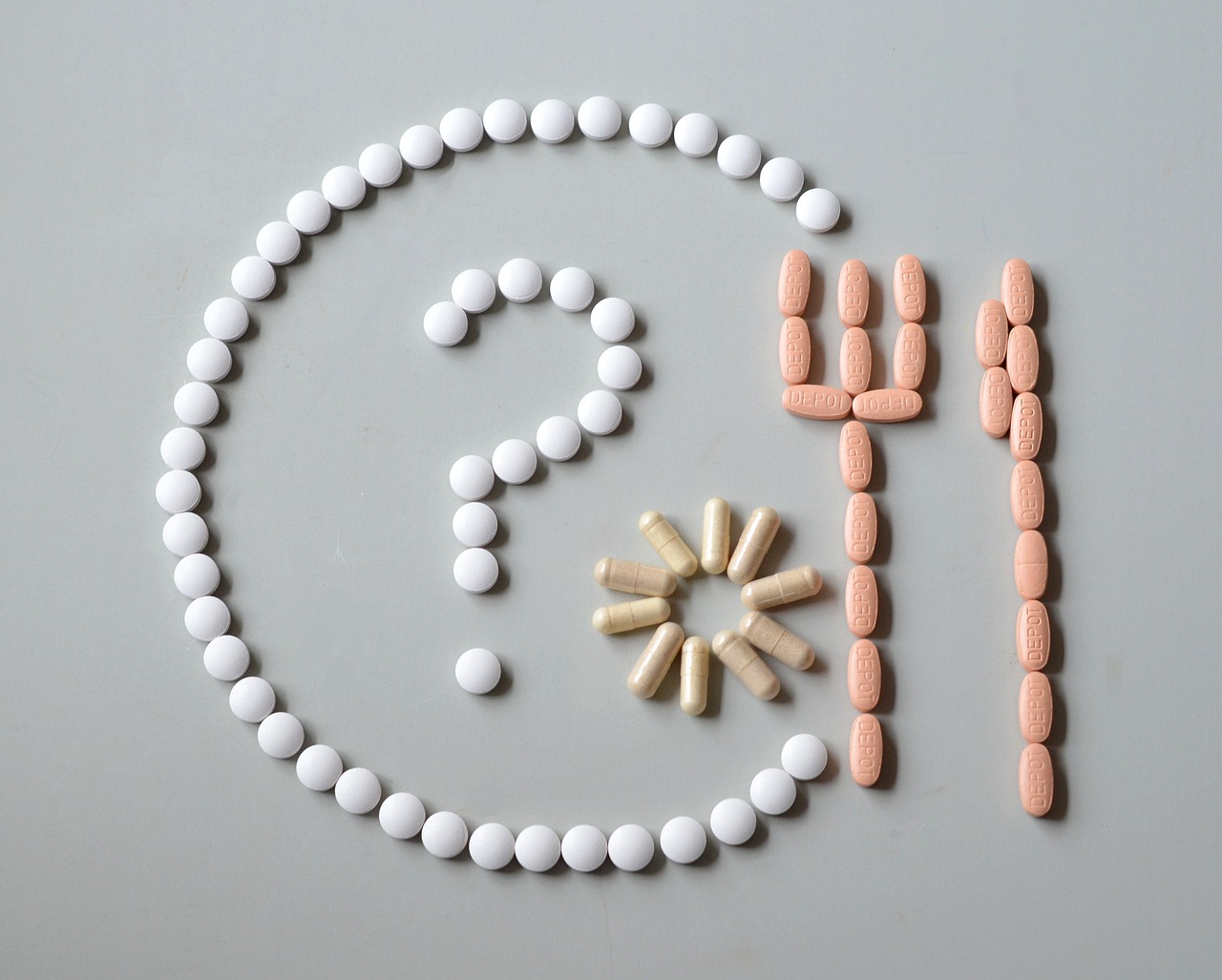
One of the most exciting aspects of nanotechnology is its potential to revolutionize drug delivery. Traditional methods often result in medications being dispersed throughout the body, leading to side effects and reduced efficacy. However, with nanotechnology, we can engineer nanocarriers—tiny particles designed to deliver drugs directly to the targeted site, such as a tumor. This targeted approach not only enhances the effectiveness of the treatment but also minimizes harmful side effects, making for a more patient-friendly experience.
As we delve deeper into the applications of nanotechnology in medicine, it becomes clear that we are on the brink of a new era in healthcare. The ability to create personalized medicine is one of the most promising advancements. Imagine a treatment plan tailored specifically to your genetic makeup! This level of customization can significantly improve therapeutic effectiveness, ensuring that patients receive the most suitable treatments while reducing the risk of adverse reactions.
However, the journey is not without its challenges. The field of cancer nanomedicine, for instance, faces hurdles such as biocompatibility issues, regulatory complexities, and the necessity for extensive clinical trials. These challenges must be addressed to harness the full potential of nanotechnology in cancer therapies and beyond.
In addition to drug delivery, nanotechnology has made remarkable strides in diagnostic imaging. Traditional imaging techniques often struggle with sensitivity and specificity, particularly in the early stages of disease. Nanotechnology enhances these techniques, allowing for the detection of diseases at much earlier stages. This capability is crucial because early detection often leads to better treatment outcomes.
As we explore the transformative role of nanotechnology in medicine, it is essential to consider the ethical implications. The integration of such powerful technology raises questions about safety, privacy, and the potential for misuse. Establishing ethical guidelines is paramount to ensure that the benefits of nanotechnology are realized without compromising patient safety or public trust.
Moreover, the regulatory framework surrounding nanomedicine is still evolving. A robust set of guidelines is necessary to ensure that nanotechnology products are safe and effective. Current regulations often lag behind technological advancements, highlighting the need for adaptive policies that can keep pace with innovation.
Finally, public perception plays a significant role in the acceptance and implementation of nanotechnology in medicine. Factors such as education, transparency, and community engagement are critical in shaping public attitudes. By fostering an informed public dialogue, we can pave the way for greater acceptance of these groundbreaking technologies.
- What is nanotechnology? Nanotechnology is the manipulation of matter at the nanoscale, typically between 1 and 100 nanometers, leading to innovative applications in various fields, including medicine.
- How does nanotechnology improve drug delivery? Nanotechnology enables the creation of nanocarriers that can deliver drugs directly to targeted sites in the body, enhancing treatment efficacy and minimizing side effects.
- What are the challenges associated with nanomedicine? Key challenges include biocompatibility, regulatory hurdles, and the need for extensive clinical trials to ensure safety and efficacy.
- How does nanotechnology enhance diagnostic imaging? Nanotechnology improves imaging techniques by increasing sensitivity and specificity, allowing for earlier disease detection.
- What ethical concerns are associated with nanotechnology in medicine? Ethical concerns include safety, privacy, and the potential for misuse, necessitating the establishment of robust ethical guidelines.
Overview of Nanotechnology in Medicine
Nanotechnology is a fascinating field that involves manipulating matter at an incredibly small scale—typically between 1 and 100 nanometers. To put that into perspective, a nanometer is one-billionth of a meter! This tiny scale opens up a world of possibilities, especially in the realm of medicine. Imagine being able to design materials and devices that can interact with biological systems at the cellular or even molecular level. This is not just science fiction; it's happening right now, and it's revolutionizing the way we approach healthcare.
The significance of nanotechnology in medicine cannot be overstated. It has paved the way for groundbreaking applications that enhance diagnostics, treatment, and prevention of diseases. For instance, in drug delivery, nanotechnology allows for the creation of nanocarriers that can transport medications directly to targeted areas in the body. This targeted approach not only improves the efficiency of treatments but also reduces side effects, as drugs can be delivered precisely where they are needed, rather than affecting the entire body.
One of the most exciting aspects of nanotechnology is its ability to improve diagnostic tools. With the help of nanoparticles, we can develop imaging agents that provide higher sensitivity and specificity. This means that diseases can be detected at much earlier stages, which is crucial for effective treatment. For example, nanoparticles can enhance the contrast in imaging techniques such as MRI or PET scans, making it easier for doctors to identify tumors or other abnormalities.
Furthermore, nanotechnology is paving the way for personalized medicine. By utilizing nanoscale materials, healthcare providers can tailor treatments based on individual patient profiles, optimizing therapeutic effectiveness and minimizing adverse reactions. This shift towards personalized medicine is akin to having a custom-made suit; it fits perfectly and meets specific needs, rather than being a one-size-fits-all solution.
However, while the potential of nanotechnology in medicine is immense, it is essential to navigate the challenges it presents. Issues such as biocompatibility, the need for extensive clinical trials, and regulatory hurdles must be addressed to ensure that these innovative solutions are safe and effective for patients. As we continue to explore the vast landscape of nanotechnology, it is crucial to maintain a balanced perspective, weighing both the benefits and the challenges that come with this groundbreaking field.

Applications of Nanotechnology in Drug Delivery
Nanotechnology has emerged as a game-changer in the realm of drug delivery, fundamentally altering how medications are administered and absorbed in the body. Imagine a tiny delivery system that can navigate through the bloodstream, pinpointing specific cells like a guided missile. This precision is not just a fantasy; it’s the reality that nanocarriers bring to the table. By using materials that operate at the nanoscale, scientists can create vehicles that transport drugs directly to the targeted area, ensuring that the medication is effective while minimizing side effects.
One of the most significant advantages of nanotechnology in drug delivery is the ability to enhance bioavailability. Traditional drug delivery methods often struggle with issues like poor solubility and rapid metabolism, which can lead to inadequate therapeutic effects. However, nanocarriers, such as liposomes, dendrimers, and nanoparticles, can encapsulate drugs, improving their stability and absorption. For instance, liposomes can encapsulate both hydrophilic and hydrophobic drugs, making them versatile tools in the pharmaceutical arsenal.
Moreover, the targeted nature of nanotechnology allows for controlled release of drugs. This means that instead of a one-size-fits-all approach, medications can be released at specific times or in response to certain triggers within the body. For example, a nanoparticle could be designed to release its payload only when it encounters the acidic environment of a tumor, effectively delivering chemotherapy directly to cancer cells while sparing healthy tissue. This not only enhances the efficacy of the treatment but also significantly reduces the debilitating side effects that many patients face.
In addition to cancer treatment, nanotechnology is making waves in treating chronic diseases such as diabetes and cardiovascular conditions. For instance, researchers are exploring nanoparticles that can deliver insulin directly to the bloodstream, providing a more effective and convenient method for diabetes management. This shift from traditional methods to nanotechnology-driven solutions represents a significant leap forward in patient care.
However, while the benefits are substantial, it's essential to acknowledge the challenges that come with these advancements. One of the primary concerns is the biocompatibility of nanomaterials. Ensuring that these materials do not provoke an adverse immune response is critical for their success in clinical applications. Additionally, the regulatory landscape for nanomedicine is still evolving, requiring thorough research and clinical trials to validate the safety and effectiveness of these innovative therapies.
In summary, the applications of nanotechnology in drug delivery are vast and varied. From enhancing bioavailability and enabling targeted therapies to providing controlled release mechanisms, the potential to improve patient outcomes is enormous. As we continue to explore this exciting field, it’s clear that nanotechnology is set to revolutionize the way we approach medication administration and disease treatment.
- What is nanotechnology in medicine? Nanotechnology in medicine refers to the application of nanoscale materials and devices to improve healthcare outcomes, including drug delivery, diagnostic imaging, and personalized medicine.
- How does nanotechnology improve drug delivery? It enhances drug delivery by allowing for targeted therapies, improved bioavailability, and controlled release of medications, reducing side effects and increasing treatment efficacy.
- What are the challenges associated with nanotechnology in drug delivery? Challenges include ensuring biocompatibility, navigating regulatory hurdles, and conducting extensive clinical trials to ensure safety and efficacy.
- Can nanotechnology be used for all types of medications? While nanotechnology shows promise for various medications, its effectiveness may vary depending on the drug's properties and the targeted condition.

Nanoformulations for Cancer Treatment
Nanoformulations are revolutionizing the way we approach cancer treatment, offering a beacon of hope in the fight against this formidable disease. Imagine a world where chemotherapy isn't just a blanket treatment, but a tailored solution that zeroes in on cancer cells while leaving healthy tissues unscathed. That's the promise of nanotechnology in oncology! By utilizing nanoparticles, researchers have developed innovative drug delivery systems that enhance the efficacy of chemotherapeutic agents. These nanoformulations can be engineered to release drugs in a controlled manner, ensuring that the medication is delivered directly to the tumor site, thereby maximizing its impact.
One of the most exciting aspects of nanoformulations is their ability to improve the bioavailability of drugs. Traditional chemotherapy often suffers from poor solubility and rapid clearance from the body, which can diminish treatment efficacy. However, with the advent of nanocarriers—such as liposomes, dendrimers, and polymeric nanoparticles—medications can be encapsulated and transported more effectively. This not only allows for higher concentrations of the drug to reach the tumor but also reduces the side effects that patients typically endure during treatment.
For instance, liposomal formulations of doxorubicin, a commonly used chemotherapeutic agent, have demonstrated improved therapeutic outcomes compared to conventional formulations. These liposomes can navigate through the bloodstream and accumulate in tumor tissues due to the enhanced permeability and retention (EPR) effect, allowing for a more potent attack on cancer cells. This targeted approach minimizes the collateral damage to healthy cells, which is a significant concern in traditional chemotherapy.
Moreover, nanoformulations can be designed for personalized medicine, tailoring treatments to the unique genetic profile of an individual's tumor. This customization is crucial because cancer is not a one-size-fits-all disease; it varies significantly from person to person. By leveraging the capabilities of nanotechnology, clinicians can analyze tumor characteristics at a molecular level and select the most effective nanoformulation for each patient, enhancing the overall success rate of cancer therapies.
However, despite the promising potential of nanoformulations, there are challenges that need to be addressed. Issues related to biocompatibility, stability, and the long-term effects of nanoparticles in the body are still under investigation. Furthermore, regulatory hurdles must be navigated to ensure that these innovative treatments meet safety standards before they can be widely adopted in clinical settings. As we continue to explore the capabilities of nanotechnology in cancer treatment, ongoing research and dialogue among scientists, clinicians, and regulatory bodies will be essential to unlock its full potential.
- What are nanoformulations? Nanoformulations are advanced drug delivery systems that utilize nanoparticles to enhance the efficacy and targeting of cancer therapies.
- How do nanoformulations improve cancer treatment? They allow for targeted delivery of drugs directly to tumor sites, improving bioavailability and minimizing side effects.
- Are there any risks associated with nanoformulations? Yes, challenges such as biocompatibility and long-term effects of nanoparticles are still being researched.
- Can nanoformulations be personalized? Absolutely! They can be tailored to fit the unique genetic profile of an individual's tumor, leading to more effective treatments.

Personalized Medicine and Nanotechnology
In the ever-evolving landscape of healthcare, personalized medicine stands out as a beacon of hope for many patients. It is all about tailoring medical treatment to the individual characteristics of each patient. Now, when we intertwine this concept with nanotechnology, the results can be nothing short of revolutionary. Imagine a world where medications are not just generic pills but are specifically designed to meet your unique biological makeup. That's the power of nanotechnology in personalized medicine!
At its core, nanotechnology allows for the manipulation of materials at an incredibly small scale—typically between 1 and 100 nanometers. This tiny scale enables scientists to create nanoformulations that can be customized to deliver drugs in a more effective manner. For instance, by using nanoparticles, we can enhance the solubility of poorly water-soluble drugs or ensure that therapeutic agents are released at the right time and at the right place within the body. This not only improves the therapeutic effectiveness but also minimizes adverse reactions, making treatments safer and more efficient.
One of the most exciting applications of this technology is in treating complex diseases like cancer. Traditional cancer treatments often come with a laundry list of side effects because they target not just the cancer cells but also healthy cells. However, with nanotechnology, we can develop targeted drug delivery systems that hone in on cancer cells specifically. This means that the chemotherapeutic agents can be encapsulated in nanoparticles that are designed to recognize and bind to cancer cells, delivering the drug directly to the tumor while sparing healthy tissue. It’s like having a guided missile that knows exactly where to strike!
Moreover, the integration of nanotechnology in personalized medicine allows for the development of biomarkers that can predict how a patient will respond to a particular treatment. These biomarkers can be embedded within nanoparticles, providing a means to monitor the effectiveness of therapies in real-time. This level of customization leads to a more informed approach to treatment, where healthcare providers can make decisions based on concrete data rather than guesswork.
Yet, while the potential is immense, there are hurdles to overcome. The journey from the lab to clinical application is fraught with challenges. Safety and efficacy must be thoroughly evaluated through rigorous testing, and the regulatory landscape is still catching up with the pace of innovation. It’s crucial that as we embrace these advanced technologies, we also prioritize patient safety and ethical considerations.
In summary, the fusion of personalized medicine and nanotechnology presents an exciting frontier in healthcare. With the ability to tailor treatments to individual needs, we are on the brink of a new era in medicine that promises not just to treat diseases but to do so in a way that is efficient, effective, and safe. As we continue to explore these possibilities, the future of personalized medicine looks brighter than ever!
- What is personalized medicine?
Personalized medicine tailors medical treatment to the individual characteristics of each patient, taking into account genetic, environmental, and lifestyle factors. - How does nanotechnology enhance personalized medicine?
Nanotechnology allows for the development of targeted drug delivery systems and customized treatments that improve efficacy and reduce side effects. - What are some challenges associated with nanotechnology in medicine?
Challenges include ensuring safety, navigating regulatory hurdles, and conducting extensive clinical trials to confirm efficacy.

Challenges in Cancer Nanomedicine
Navigating the landscape of cancer nanomedicine is like sailing through uncharted waters; while the potential is vast and exciting, there are significant challenges that researchers and clinicians must face. One of the primary hurdles is biocompatibility. Nanoparticles, while effective in targeting cancer cells, can sometimes provoke unintended immune responses. This unpredictability can lead to adverse reactions in patients, which raises critical questions about safety. Imagine trying to introduce a new friend to your circle; if they don’t get along with the group, it can create tension. Similarly, if nanocarriers don’t harmonize with the body, the results can be detrimental.
Another significant challenge is the regulatory landscape. The field of nanomedicine is evolving rapidly, often outpacing existing regulations designed to ensure patient safety. Regulatory bodies are tasked with evaluating new technologies, but the unique properties of nanomaterials complicate this process. For instance, the same nanoparticle might behave differently depending on its size, shape, and surface characteristics. This variability means that a one-size-fits-all approach to regulation is inadequate. As a result, extensive clinical trials are necessary to gather sufficient data on safety and efficacy, which can be both time-consuming and expensive.
Moreover, the manufacturing process for nanomedicine products poses its own set of challenges. Producing nanoparticles with consistent quality and characteristics is crucial for ensuring their effectiveness. Any variation in the production process can lead to differences in how the nanoparticles interact with cancer cells, potentially undermining treatment outcomes. Picture baking a cake; if you alter the ingredients or the baking time even slightly, the final product can turn out drastically different.
Lastly, there is the challenge of patient education and acceptance. Many patients are understandably cautious about new treatments, especially those involving nanotechnology. There is often a lack of understanding about how these advanced therapies work, which can lead to skepticism. To bridge this gap, healthcare providers need to engage in open, informative conversations with patients about the benefits and risks associated with nanomedicine. Building trust is essential, and this can only be achieved through transparency and education.
In summary, while the prospects of cancer nanomedicine are incredibly promising, addressing these challenges is crucial for the successful integration of nanotechnology into clinical practice. As researchers continue to innovate and refine these technologies, ongoing dialogue among scientists, regulatory bodies, and the public will be essential to ensure that the benefits of nanomedicine can be fully realized.
- What is cancer nanomedicine?
Cancer nanomedicine refers to the use of nanotechnology to diagnose, treat, and prevent cancer. It involves the application of nanomaterials to enhance drug delivery and improve the efficacy of treatments.
- What are the advantages of using nanotechnology in cancer treatment?
Nanotechnology allows for targeted delivery of drugs, reducing side effects and improving treatment outcomes. It can also enhance imaging techniques, enabling earlier detection of cancer.
- What challenges does cancer nanomedicine face?
Challenges include biocompatibility issues, regulatory hurdles, manufacturing consistency, and patient acceptance.
- How does regulatory approval work for nanomedicine?
Regulatory approval for nanomedicine involves rigorous evaluation of safety and efficacy, often requiring extensive clinical trials due to the unique properties of nanomaterials.

Nanotechnology in Diagnostic Imaging
Advancements in nanotechnology have ushered in a new era in the field of diagnostic imaging, fundamentally changing the way we detect and diagnose diseases. Imagine being able to visualize biological processes at the molecular level; this is what nanotechnology offers. By utilizing nanoparticles, healthcare professionals can achieve unprecedented sensitivity and specificity, enabling them to spot diseases much earlier than traditional methods allow. This capability is crucial, especially in conditions like cancer, where early detection can significantly influence treatment outcomes.
Nanoparticles, which are typically 1 to 100 nanometers in size, can be engineered to target specific cells or tissues. This means that they can carry imaging agents directly to the areas of interest, enhancing the quality of the images obtained. For instance, gold nanoparticles are often used in imaging due to their unique optical properties. They can scatter light in a way that improves contrast in imaging techniques like computed tomography (CT) and magnetic resonance imaging (MRI). This targeted approach not only improves the accuracy of diagnoses but also reduces the amount of contrast agent needed, minimizing potential side effects for patients.
Furthermore, the integration of nanotechnology in diagnostic imaging allows for the development of multimodal imaging techniques. These techniques combine different imaging modalities, such as PET, MRI, and ultrasound, into a single platform. This synergy enhances the diagnostic capabilities, providing a more comprehensive view of the patient's condition. For example, a nanoparticle can be designed to emit signals detectable by both MRI and PET scans, allowing for a more detailed understanding of tumor biology and behavior.
However, it's not just about the technology itself; the implications of these advancements are profound. With improved imaging techniques, healthcare providers can make better-informed decisions, leading to personalized treatment plans that cater specifically to the patient's needs. This shift towards personalized medicine is a game-changer, as it enhances the effectiveness of treatments and reduces the likelihood of adverse reactions.
Despite these exciting developments, challenges remain. The complexity of biological systems can sometimes lead to unpredictable interactions between nanoparticles and biological tissues. Additionally, the regulatory landscape for nanotechnology in medicine is still evolving, and ensuring that these new imaging techniques are safe and effective requires rigorous testing and validation. The future of nanotechnology in diagnostic imaging holds great promise, but it is vital for researchers, clinicians, and regulatory bodies to work together to navigate these challenges.
In summary, the role of nanotechnology in diagnostic imaging is transforming the healthcare landscape. With its ability to enhance sensitivity and specificity, facilitate early disease detection, and enable personalized treatment approaches, nanotechnology is not just a tool; it is a revolution in how we understand and interact with human health.
- What is nanotechnology in diagnostic imaging?
Nanotechnology in diagnostic imaging involves using nanoparticles to enhance the quality and accuracy of medical imaging techniques, allowing for earlier detection of diseases. - How do nanoparticles improve imaging techniques?
Nanoparticles can be engineered to target specific tissues, increasing the contrast and clarity of images obtained through methods like MRI and CT scans. - Are there any risks associated with nanotechnology in medicine?
While nanotechnology holds great promise, there are potential risks related to biocompatibility and the need for extensive clinical testing to ensure safety. - What are multimodal imaging techniques?
Multimodal imaging techniques combine different imaging methods to provide a more comprehensive view of a patient's condition, improving diagnostic accuracy.

Ethical Considerations in Nanomedicine
The integration of nanotechnology into medicine is not just a scientific leap; it also brings forth a myriad of ethical considerations that must be addressed to ensure responsible application. As we stand on the brink of revolutionary advancements, it's crucial to reflect on the implications of these technologies on society. One of the primary concerns revolves around safety. How do we ensure that nanomaterials used in treatments do not pose unforeseen risks to patients or the environment? The nanoscale manipulation of materials can lead to properties that are not fully understood, necessitating rigorous testing and evaluation.
Moreover, privacy issues arise, particularly in personalized medicine. With treatments tailored to individual genetic profiles, how do we safeguard sensitive patient information? As we gather data to create these personalized therapies, the potential for misuse of this information becomes a pressing concern. Patients must be assured that their data is handled with the utmost care and confidentiality.
Another significant ethical dilemma involves access to treatments. As nanotechnology paves the way for cutting-edge therapies, we must ask ourselves: will these advancements be available to everyone, or will they deepen the existing healthcare disparities? The high costs associated with developing and implementing nanomedicine could limit access for underprivileged populations, raising questions about equity in healthcare. It's essential for stakeholders to consider strategies that ensure these innovations benefit all segments of society.
Furthermore, the potential for misuse of nanotechnology in medicine cannot be overlooked. Like any powerful tool, nanotechnology can be wielded for harmful purposes, such as creating biological weapons or enhancing unethical practices. This reality emphasizes the need for clear ethical guidelines and regulations to govern the research and application of nanomedicine.
In light of these considerations, establishing a robust regulatory framework is essential. This framework should not only focus on the scientific and technical aspects but also incorporate ethical principles that prioritize patient safety, privacy, and equitable access. Here’s a brief overview of the key ethical principles that should guide nanomedicine:
| Ethical Principle | Description |
|---|---|
| Safety | Ensuring that nanomaterials used in treatments do not pose risks to patients or the environment. |
| Privacy | Protecting sensitive patient data, especially in personalized medicine. |
| Equity | Guaranteeing that advancements in nanomedicine are accessible to all, regardless of socioeconomic status. |
| Accountability | Establishing clear guidelines to prevent misuse of nanotechnology. |
As we navigate the complexities of nanotechnology in medicine, it is imperative that we engage in open discussions about these ethical considerations. By fostering a culture of transparency and accountability, we can harness the potential of nanomedicine while safeguarding the rights and well-being of individuals and communities.
- What is nanomedicine? Nanomedicine refers to the application of nanotechnology in the field of medicine, including drug delivery, diagnostics, and treatment.
- What are the ethical concerns related to nanotechnology? Key concerns include safety, privacy, equitable access, and the potential for misuse of technology.
- How can we ensure equitable access to nanomedicine? Strategies such as policy-making and community engagement are essential to ensure that advancements benefit all segments of society.
- What role do regulations play in nanomedicine? Regulations are crucial for ensuring the safety, efficacy, and ethical application of nanotechnology in healthcare.

Regulatory Framework for Nanomedicine
As the field of nanomedicine continues to evolve, establishing a robust regulatory framework becomes paramount to ensure the safety and efficacy of nanotechnology-based products. Regulatory bodies around the world, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), are tasked with the critical role of overseeing the development and approval of these innovative therapies. However, the unique characteristics of nanomaterials—such as their size, shape, and surface properties—often complicate the traditional regulatory processes.
One of the primary challenges is that nanomedicine does not fit neatly into existing categories of medical products. For instance, a drug that utilizes nanoparticles for delivery might need to be assessed differently than a conventional drug. This necessitates a tailored approach to regulation, which includes rigorous testing for biocompatibility, toxicity, and long-term effects on human health and the environment.
Moreover, the regulatory landscape is further complicated by the rapid pace of technological advancement in nanotechnology. As new applications emerge, regulatory agencies must adapt by developing guidelines and standards that address the specific risks and benefits associated with nanomedicine. This includes establishing clear definitions and classifications for nanomaterials, which is essential for consistent regulatory oversight.
For example, the FDA has issued guidance documents that outline the necessary preclinical and clinical data required for the approval of nanomedicine products. These guidelines emphasize the importance of understanding the pharmacokinetics and pharmacodynamics of nanomedicines, which are critical for predicting how these products will behave in the human body.
| Regulatory Body | Key Responsibilities |
|---|---|
| U.S. Food and Drug Administration (FDA) | Oversees the approval of drugs and biologics, including those utilizing nanotechnology. |
| European Medicines Agency (EMA) | Regulates medicinal products in the EU, ensuring safety and efficacy. |
| National Institute of Health (NIH) | Funds research and provides guidelines for nanotechnology in health. |
In addition to regulatory bodies, there is a growing need for collaboration between researchers, industry stakeholders, and regulators to foster an environment of innovation while maintaining safety standards. By engaging in open dialogue and sharing information, these parties can work together to address the complexities of nanomedicine regulation.
Furthermore, ethical considerations must also be woven into the regulatory framework. Issues such as patient consent, privacy, and the potential for misuse of nanotechnology raise important questions that regulatory bodies must address. Establishing ethical guidelines will not only enhance public trust but also promote responsible research and application of nanomedicine.
As we look to the future, it is clear that a dynamic and responsive regulatory framework is essential for the successful integration of nanotechnology into medicine. By prioritizing safety, efficacy, and ethical considerations, we can harness the full potential of nanomedicine to transform healthcare and improve patient outcomes.
- What is nanomedicine? Nanomedicine is the application of nanotechnology for medical purposes, including drug delivery, diagnostics, and treatment.
- Why is regulation important in nanomedicine? Regulation ensures that nanomedicine products are safe and effective, protecting patient health and fostering public trust.
- What challenges do regulators face with nanomedicine? Regulators must adapt existing frameworks to address the unique properties of nanomaterials and their potential risks.
- How can the public be involved in the regulatory process? Public engagement through education and transparency can help shape policies and promote acceptance of nanomedicine.

Public Perception and Acceptance
The landscape of nanotechnology in medicine is not just shaped by scientific advancements; it is also profoundly influenced by how the public perceives these innovations. Imagine a world where tiny particles can deliver medication directly to a tumor, minimizing side effects and maximizing effectiveness. Sounds like science fiction, right? Yet, this is the reality that nanotechnology promises. However, the journey from discovery to acceptance is often fraught with skepticism and concern.
One of the primary factors influencing public perception is the level of understanding about what nanotechnology entails. Many people are unaware of its potential benefits, leading to misconceptions. For instance, some may equate nanotechnology with risks associated with synthetic chemicals or genetically modified organisms. To bridge this knowledge gap, educational initiatives are crucial. The more informed the public is about the science behind nanotechnology, the more likely they are to embrace its applications in healthcare.
Moreover, the media plays a significant role in shaping public attitudes. Sensational headlines can often lead to fear and misunderstanding. When the media focuses on the potential dangers of nanotechnology without adequately addressing its benefits, it can create a climate of fear. This highlights the importance of responsible reporting and the need for scientists and healthcare professionals to engage with the media effectively.
Another critical aspect to consider is the ethical implications surrounding nanotechnology. People are naturally concerned about safety and privacy when it comes to new medical technologies. Questions arise, such as: “Will these nanoparticles remain in my body?” or “How will my personal health data be protected?” Addressing these concerns transparently is essential for fostering trust. For instance, clear communication about the safety measures in place during the development and application of nanomedicine can help alleviate fears.
Interestingly, public acceptance can also be influenced by cultural factors. Different societies have varying levels of trust in science and technology. In some cultures, there is a strong belief in traditional medicine, which can lead to resistance against modern techniques like nanotechnology. Understanding these cultural nuances is vital for researchers and policymakers aiming to promote nanomedicine globally.
In summary, public perception of nanotechnology in medicine is a complex interplay of knowledge, media representation, ethical considerations, and cultural beliefs. To enhance acceptance, it is crucial to prioritize education and transparent communication. By doing so, we can pave the way for a future where nanotechnology is not only accepted but celebrated for its transformative potential in healthcare.
- What is nanotechnology? Nanotechnology involves manipulating matter at the nanoscale, typically between 1 and 100 nanometers, to create new materials and devices with unique properties.
- How does nanotechnology improve drug delivery? Nanotechnology enables targeted drug delivery, allowing medications to be delivered directly to affected areas, which enhances efficacy and reduces side effects.
- Are there risks associated with nanotechnology in medicine? As with any emerging technology, there are potential risks, including safety concerns and ethical implications, which need to be addressed through rigorous testing and transparent communication.
- How can the public become more informed about nanotechnology? Engaging in educational programs, reading credible sources, and participating in community discussions can help increase public understanding and acceptance of nanotechnology.
Frequently Asked Questions
- What is nanotechnology in medicine?
Nanotechnology in medicine refers to the manipulation of matter at the nanoscale, which is about 1 to 100 nanometers. This innovative approach allows for the development of advanced medical applications, including targeted drug delivery systems, improved diagnostic tools, and personalized therapies that can significantly enhance patient outcomes.
- How does nanotechnology improve drug delivery?
Nanotechnology enhances drug delivery by using nanocarriers that can transport medications directly to the target site in the body. This targeted approach increases the bioavailability of drugs, allowing for lower doses and reduced side effects. It's like having a precision-guided missile that strikes exactly where it needs to without causing collateral damage!
- What role does nanotechnology play in cancer treatment?
Nanoformulations in cancer treatment allow for the direct delivery of chemotherapy drugs to tumor cells, which minimizes damage to surrounding healthy tissue. This targeted therapy not only improves the efficacy of the treatment but also reduces the unpleasant side effects often associated with traditional chemotherapy.
- Are there challenges associated with cancer nanomedicine?
Yes, despite its promise, cancer nanomedicine faces several challenges, including issues of biocompatibility, regulatory hurdles, and the need for extensive clinical trials. These factors are crucial to ensure that nanomedicine products are both safe and effective for patient use.
- How does nanotechnology enhance diagnostic imaging?
Advancements in nanotechnology have led to the development of imaging agents that provide higher sensitivity and specificity. This means diseases can be detected at much earlier stages, which is vital for effective treatment. Think of it as upgrading from a regular camera to a high-definition one that captures every detail!
- What ethical concerns are associated with nanomedicine?
The use of nanotechnology in medicine raises several ethical issues, including safety concerns, privacy implications, and the potential for misuse. Establishing strong ethical guidelines is essential to navigate these challenges and promote responsible research and application in the field.
- What is the regulatory framework for nanomedicine?
A robust regulatory framework is crucial for ensuring the safety and efficacy of nanomedicine products. Current regulations are evolving to address the unique challenges posed by nanotechnology, and there is a growing need for adaptive policies that can keep pace with rapid advancements in this field.
- How does public perception affect nanotechnology in medicine?
Public perception plays a significant role in the acceptance and implementation of nanotechnology in medicine. Factors such as education, transparency, and clear communication about the benefits and risks can greatly influence how the public views and embraces these innovative medical solutions.



















