A Deep Dive into AI Guided Surgery
In recent years, the landscape of medicine has been transformed by the advent of artificial intelligence, particularly in the field of surgery. Imagine a world where surgical procedures are not only more precise but also safer and faster—this is the reality that AI is helping to create. From enhancing the surgeon's capabilities to providing real-time data analysis, AI is revolutionizing how surgeries are performed. But what does this mean for patients and healthcare providers alike? As we delve deeper into this topic, we will explore the myriad ways AI is reshaping surgical techniques, the technologies at play, and the ethical considerations that must be addressed.
The journey of surgical techniques has been nothing short of remarkable. Historically, surgeries were rudimentary at best, often involving significant risks and lengthy recovery periods. Over the years, we have witnessed a series of pivotal milestones, such as the introduction of anesthesia in the 19th century, which revolutionized patient comfort, and the development of antiseptic methods that drastically reduced infection rates. Fast forward to the late 20th century, and we see the rise of minimally invasive procedures, which have transformed patient care. Today, we stand on the brink of a new era, one defined by the integration of AI technologies that promise to enhance surgical precision and improve patient outcomes dramatically.
At the heart of this transformation are various AI technologies, including machine learning and robotics. These innovations are not just buzzwords; they are actively being utilized in surgical practices to improve efficiency and accuracy. For instance, machine learning algorithms can analyze vast amounts of data to predict patient outcomes, assist in diagnostics, and even recommend treatment plans tailored to individual needs. On the other hand, robotic systems provide surgeons with enhanced dexterity and control, allowing them to perform complex procedures with remarkable precision. The marriage of these technologies is paving the way for a future where surgeries are safer, faster, and more effective.
Robotic-assisted surgery represents a significant leap forward in surgical capabilities. Imagine a surgeon operating from a console, controlling robotic arms with precision that surpasses human capabilities. This technology enhances the surgeon's ability to perform intricate maneuvers that would be challenging with traditional methods. As a result, patients benefit from improved outcomes and faster recovery times. But what exactly are the advantages of using robotic systems in surgery?
Robotic systems offer a multitude of benefits that can significantly improve the surgical experience for patients. Some of the key advantages include:
- Minimally Invasive Procedures: Smaller incisions lead to reduced pain and scarring.
- Reduced Blood Loss: Enhanced precision minimizes tissue damage.
- Shorter Hospital Stays: Patients often go home sooner, allowing for quicker recovery.
Despite the advantages, robotic-assisted surgeries are not without their challenges. The high cost of robotic systems can be a significant barrier for many healthcare facilities. Additionally, the technical complexities involved require specialized training for surgeons, which can be a time-consuming process. As we continue to explore the integration of AI in surgery, it's essential to address these challenges to maximize the potential of robotic systems.
Machine learning is revolutionizing surgical decision-making by providing surgeons with data-driven insights. Imagine having a virtual assistant that can analyze patient data in real-time, offering recommendations based on past cases and outcomes. This capability not only improves diagnostic accuracy but also enhances treatment planning, allowing surgeons to make more informed decisions during operations. The potential for machine learning to reduce errors and improve patient safety is immense, making it an invaluable tool in the operating room.
As we embrace the benefits of AI in surgery, we must also confront the ethical implications that arise. Issues such as data privacy, accountability, and the potential for bias in AI algorithms are critical concerns that cannot be overlooked. For instance, how do we ensure that patient data is protected when utilizing AI technologies? Moreover, who is responsible if an AI system makes a mistake during a surgical procedure? These questions highlight the need for robust ethical frameworks as we navigate this new landscape.
Informed consent becomes increasingly complex in the context of AI-guided surgeries. Patients must understand how AI will be used in their treatment and the implications it entails. Transparency is key—healthcare providers need to communicate clearly about the role of AI, ensuring that patients are fully aware of the technologies being employed in their care.
As AI technologies become more integrated into surgical procedures, the legal and ethical responsibilities of healthcare providers must be clearly defined. If an AI system fails, who is liable? The surgeon, the hospital, or the AI developers? These questions are pivotal in ensuring patient safety and maintaining care standards in an increasingly automated environment.
Q: How does AI improve surgical outcomes?
A: AI enhances surgical outcomes by providing real-time data analysis, improving precision, and assisting in decision-making during procedures.
Q: Are there risks associated with AI in surgery?
A: Yes, risks include data privacy concerns, potential biases in AI algorithms, and the need for specialized training for healthcare providers.
Q: What are the benefits of robotic-assisted surgery?
A: Benefits include minimally invasive procedures, reduced blood loss, and shorter recovery times for patients.
Q: How can patients ensure they understand AI's role in their treatment?
A: Patients should engage in open discussions with their healthcare providers to clarify how AI will be used in their surgical procedures.

The Evolution of Surgical Techniques
The journey of surgical techniques is nothing short of fascinating, marked by a series of transformative milestones that have revolutionized the way we approach surgery today. From the rudimentary practices of ancient civilizations to the sophisticated and precise methods we employ now, surgery has evolved dramatically over the centuries. In ancient times, surgery was often a last resort, performed without anesthesia and under unsanitary conditions. Imagine a time when a surgeon's toolkit consisted of crude instruments made from stone or bronze, and the risks of infection were alarmingly high!
Fast forward to the 19th century, and we see a pivotal moment in surgical history with the introduction of anesthesia. This groundbreaking development not only made surgeries more bearable for patients but also opened the door to more complex procedures. Surgeons could now operate with greater precision and confidence, knowing that their patients were not in excruciating pain. The discovery of antiseptics soon followed, drastically reducing the rates of post-operative infections and paving the way for safer surgeries.
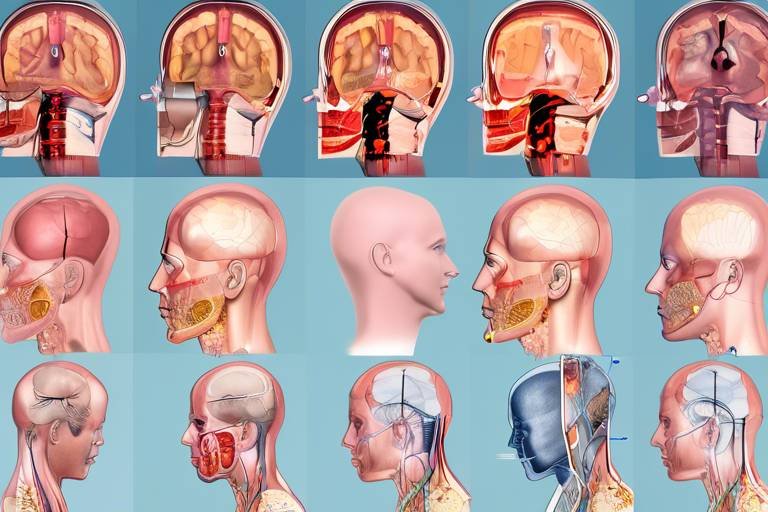
As we progressed into the 20th century, the advent of advanced imaging technologies, such as X-rays and MRIs, completely transformed the surgical landscape. Surgeons could now visualize the internal structures of the body in unprecedented detail, allowing for more accurate diagnoses and targeted interventions. This era also saw the rise of laparoscopic surgery, a minimally invasive technique that utilizes small incisions and specialized instruments, leading to quicker recovery times and less trauma for patients.
The integration of technology in surgery has reached new heights with the introduction of robotic systems and artificial intelligence. These innovations represent the culmination of centuries of surgical evolution, combining human skill with machine precision. Robotic-assisted surgeries allow for enhanced dexterity and control, enabling surgeons to perform intricate procedures with unprecedented accuracy. For instance, a robotic arm can replicate the surgeon's movements with remarkable fidelity, minimizing the margin for error.
To better understand this evolution, let’s look at a timeline of key surgical advancements:
| Year | Milestone |
|---|---|
| 3000 BC | Earliest known surgical practices in ancient Egypt. |
| 1846 | Introduction of anesthesia in surgery. |
| 1867 | Joseph Lister promotes antiseptic techniques. |
| 1980s | Emergence of laparoscopic surgery. |
| 2000s | Advancements in robotic-assisted surgical systems. |
Today, we stand at the precipice of a new era in surgery, where AI and machine learning are set to further enhance surgical techniques. These technologies not only assist in pre-operative planning but also provide real-time data during surgery, allowing for more informed decisions. The evolution of surgical techniques is a testament to human ingenuity and perseverance, and as we embrace the future, the potential for improved patient outcomes and surgical precision is truly exciting!

AI Technologies in Surgery
Artificial Intelligence (AI) is revolutionizing the field of surgery, propelling it into an era of enhanced precision and efficiency. Imagine a world where surgical outcomes are not just improved but optimized through the use of intelligent algorithms and robotic systems. This is not a distant dream; it’s happening right now. AI technologies, such as machine learning and robotics, are being integrated into surgical practices, allowing surgeons to perform complex procedures with unprecedented accuracy.
At the heart of this transformation is machine learning, a subset of AI that enables systems to learn from data and make informed predictions. In surgical settings, machine learning algorithms analyze vast amounts of patient data—everything from medical histories to real-time vitals—helping surgeons make better decisions. For instance, these algorithms can identify patterns that humans might overlook, leading to improved diagnostic accuracy and tailored treatment plans. Imagine a surgeon being equipped with a virtual assistant that can sift through a patient's entire medical history in seconds, providing insights that can significantly influence surgical strategies.
Another groundbreaking technology is robotic-assisted surgery, which is changing the way operations are performed. Robotic systems, equipped with high-definition cameras and precision instruments, allow surgeons to perform minimally invasive procedures with enhanced dexterity. This technology minimizes the physical strain on surgeons and reduces the trauma experienced by patients. The precision of robotic systems means smaller incisions, less blood loss, and quicker recovery times. It's like having a superpower in the operating room, where every movement is calculated and executed with perfection.
To illustrate the impact of AI technologies in surgery, consider the following table that outlines the key AI applications:
| AI Technology | Application in Surgery | Benefits |
|---|---|---|
| Machine Learning | Data analysis for diagnosis and treatment planning | Improved accuracy, personalized patient care |
| Robotic Surgery | Minimally invasive procedures | Reduced recovery time, less pain |
| AI Imaging | Enhanced imaging techniques for better visualization | Increased precision in targeting surgical sites |
While the benefits of AI technologies in surgery are compelling, it’s essential to recognize that they come with their own set of challenges. For instance, the integration of these technologies requires substantial investment and training. Surgeons must become adept at using these advanced tools, which can be daunting given the steep learning curve. Moreover, the reliance on AI raises questions about the human element in surgery. Can we trust machines to make decisions that could impact lives? This brings us to a crucial aspect of AI in surgery—balancing technology with human expertise.
As we venture further into this AI-driven future, it's clear that the landscape of surgery is changing. The synergy between human skill and artificial intelligence holds the promise of not just enhancing surgical procedures but also improving patient outcomes. With ongoing advancements, we can expect AI to play an even more significant role in surgeries, making the impossible possible and ensuring that patients receive the best care available.
- What is AI in surgery? AI in surgery refers to the use of artificial intelligence technologies, such as machine learning and robotics, to assist surgeons in performing operations with greater precision and efficiency.
- How does robotic-assisted surgery work? Robotic-assisted surgery involves the use of robotic systems that provide surgeons with enhanced control and visualization during procedures, leading to minimally invasive surgeries.
- What are the benefits of using AI in surgery? Benefits include improved diagnostic accuracy, reduced recovery times, minimized blood loss, and overall better patient outcomes.
- Are there risks associated with AI in surgery? Yes, challenges include high costs, the need for specialized training, and ethical considerations regarding accountability and patient consent.

Robotic-Assisted Surgery
Robotic-assisted surgery is revolutionizing the way surgeons operate, bringing a new level of precision and control to the operating room. Imagine a highly skilled surgeon, but instead of using their hands directly, they are controlling robotic arms that perform the surgery with incredible accuracy. This technology is not just a gimmick; it represents a significant leap forward in surgical techniques, allowing for minimally invasive procedures that drastically reduce recovery times and improve patient outcomes.
At the heart of robotic-assisted surgery is a system that combines advanced imaging, computer technology, and robotics to assist surgeons in performing complex procedures. These systems provide a 3D view of the surgical site, allowing for enhanced visualization that is crucial during intricate operations. For instance, in procedures like prostatectomies or hysterectomies, the robotic system enables surgeons to operate through small incisions, which is a game-changer for patient recovery. Instead of lengthy hospital stays, many patients are able to return home the same day or the next, with significantly less pain and scarring.
The benefits of robotic systems extend beyond just the surgery itself. Surgeons who utilize these systems report increased confidence in their ability to perform complex tasks, knowing they have the support of advanced technology. This confidence can translate into better surgical outcomes. However, it’s essential to acknowledge that the integration of robotics into surgery is not without its challenges. The initial costs of acquiring robotic systems can be daunting for many medical facilities. Additionally, there is a steep learning curve associated with mastering these technologies, necessitating specialized training for surgeons and their teams.
Moreover, while robotic-assisted surgery has proven to be effective, it does not replace the surgeon's expertise. Instead, it enhances their capabilities, allowing them to focus on critical decision-making while the robotic system handles the more intricate aspects of the procedure. As we look to the future of robotic-assisted surgery, we can expect ongoing advancements in technology that will further improve the precision and efficiency of surgical procedures.
In summary, robotic-assisted surgery represents a remarkable evolution in the field of medicine. With its ability to enhance surgical precision, reduce recovery times, and improve patient outcomes, it is clear that this technology is here to stay. As more healthcare providers adopt robotic systems, we can anticipate a future where complex surgeries are performed with even greater accuracy and safety, ushering in a new era of surgical excellence.
- What is robotic-assisted surgery?
Robotic-assisted surgery involves the use of robotic systems to aid surgeons in performing complex procedures with enhanced precision and control. - What are the benefits of robotic-assisted surgery?
The benefits include minimally invasive procedures, reduced blood loss, shorter recovery times, and improved surgical outcomes. - Are there any risks associated with robotic-assisted surgery?
As with any surgical procedure, there are risks involved, but robotic-assisted surgery is generally considered safe when performed by trained professionals. - How does robotic surgery differ from traditional surgery?
Robotic surgery uses robotic systems for enhanced precision, while traditional surgery relies solely on the surgeon's hands.

Benefits of Robotic Systems
Robotic systems have revolutionized the landscape of surgical procedures, bringing forth a myriad of benefits that enhance both the surgeon's capabilities and the patient's experience. One of the most significant advantages is the ability to perform minimally invasive surgeries. Unlike traditional methods that often require large incisions, robotic systems enable surgeons to operate through tiny openings. This not only reduces the trauma to the body but also leads to quicker recovery times for patients. Imagine being able to go home the same day after a major surgery—sounds like a dream, right? Well, it's becoming a reality thanks to these advanced technologies.
Another remarkable benefit is the enhanced precision that robotic systems provide. Surgeons can manipulate robotic instruments with unparalleled accuracy, often exceeding what is possible with the human hand alone. This precision is particularly crucial in delicate surgeries, such as those involving the heart or brain, where even the slightest error can have significant consequences. It’s like having a superpower that allows surgeons to navigate through complex anatomy with ease.
Additionally, robotic systems contribute to reduced blood loss during procedures. The precision of robotic instruments leads to less damage to surrounding tissues and blood vessels, which not only minimizes the risk of complications but also enhances the overall safety of the surgery. Patients often experience shorter hospital stays as a result, allowing them to return to their daily lives faster. This efficiency can be a game-changer for both the healthcare system and patients, reducing the burden on hospitals and improving patient satisfaction.
Moreover, robotic-assisted surgeries often lead to less postoperative pain. With smaller incisions and less trauma to the body, patients report a more manageable recovery experience. This means fewer pain medications are required, which is a significant plus for patient comfort and safety. It’s like trading in a clunky old car for a sleek, efficient model that gets you where you need to go without the bumps along the way.
In summary, the benefits of robotic systems in surgery are vast and impactful. They not only enhance surgical precision and reduce recovery times but also improve patient outcomes significantly. As technology continues to evolve, we can only anticipate even greater advancements in this field, making surgeries safer and more effective than ever before.
- What types of surgeries can be performed using robotic systems?
Robotic systems can be used in various surgical specialties, including urology, gynecology, cardiothoracic surgery, and general surgery. Procedures such as prostatectomies, hysterectomies, and heart valve repairs are commonly performed using robotic assistance.
- Are robotic surgeries safe?
Yes, robotic surgeries are generally considered safe. They have been shown to reduce complications, blood loss, and recovery time. However, as with any surgical procedure, there are risks involved, and it is essential to discuss these with your healthcare provider.
- How does recovery compare between traditional and robotic surgery?
Patients who undergo robotic surgery typically experience a faster recovery compared to those who have traditional open surgery. This is due to the minimally invasive nature of robotic procedures, which leads to less postoperative pain and quicker return to normal activities.

Challenges of Robotic Surgery
While robotic surgery has revolutionized the field of medicine, offering incredible precision and control, it is not without its challenges. One of the primary hurdles is the high cost associated with robotic surgical systems. These advanced machines can cost millions of dollars, making it difficult for many healthcare facilities, especially smaller hospitals, to invest in this technology. This financial barrier can limit access to cutting-edge surgical options for patients who might benefit from them.
Furthermore, the technical complexities involved in operating robotic systems present another significant challenge. Surgeons must undergo extensive training to become proficient in using these sophisticated tools. This requirement can lead to a steep learning curve, and not all surgeons may feel comfortable transitioning from traditional methods to robotic-assisted techniques. The need for specialized training can also create disparities in the availability of skilled practitioners, meaning that some patients may not have access to the best surgical options.
Additionally, there are concerns regarding patient safety and the potential for complications during robotic surgeries. While robotic systems are designed to enhance accuracy, they are still reliant on human operation. Any error or misjudgment on the part of the surgeon can lead to serious consequences, highlighting the importance of experience and skill in robotic-assisted procedures. Moreover, technical malfunctions or software issues can introduce unforeseen risks during surgery, raising questions about the reliability of these systems.
Another challenge lies in the integration of robotic systems into existing surgical protocols. Healthcare facilities may struggle to adapt their workflows and processes to accommodate this new technology, which can lead to inefficiencies and confusion in the operating room. The collaboration between surgical teams and robotic systems requires a well-coordinated effort, and any breakdown in communication can jeopardize patient outcomes.
In conclusion, while robotic surgery holds immense promise for improving surgical outcomes, it is essential to address these challenges. By investing in training, ensuring equitable access to technology, and maintaining rigorous safety protocols, the medical community can work towards maximizing the benefits of robotic-assisted procedures while minimizing the associated risks.
- What are the main advantages of robotic surgery? Robotic surgery offers enhanced precision, reduced blood loss, and shorter recovery times compared to traditional surgical methods.
- Are there risks associated with robotic surgery? Yes, risks include potential technical malfunctions, reliance on the surgeon's skill, and the possibility of complications during the procedure.
- How much does robotic surgery cost? The cost can vary significantly, often ranging from several thousand to millions of dollars depending on the procedure and healthcare facility.
- Is specialized training required for surgeons using robotic systems? Absolutely, surgeons must undergo specific training to effectively and safely operate robotic surgical systems.

Machine Learning in Surgical Decision-Making
When it comes to the world of surgery, the stakes couldn't be higher. Every decision made in the operating room can significantly impact patient outcomes. This is where machine learning steps in, revolutionizing the way surgeons approach their craft. Imagine having a virtual assistant that can analyze vast amounts of data in seconds, providing insights that a human might overlook. That's the power of machine learning in surgical decision-making.
Machine learning algorithms are designed to learn from data, improving their accuracy and predictions over time. They analyze historical patient data, surgical outcomes, and even real-time information during procedures. This capability allows for enhanced diagnostic accuracy and treatment planning. For instance, these algorithms can identify patterns in patient data that suggest the best surgical approach, helping surgeons make informed decisions tailored to each individual.
One of the most exciting aspects of machine learning in surgery is its ability to assist in predictive analytics. By examining previous cases, algorithms can forecast potential complications, enabling surgeons to prepare for challenges before they arise. This proactive approach is akin to having a seasoned navigator on a treacherous journey, guiding the surgeon through potential pitfalls.
Consider the following ways machine learning enhances surgical decision-making:
- Enhanced Diagnostics: Algorithms can analyze imaging data, such as MRIs and CT scans, with remarkable precision, identifying anomalies that might be missed by the human eye.
- Personalized Treatment Plans: By considering a patient's unique medical history and genetic information, machine learning can help create customized surgical strategies.
- Real-Time Data Analysis: During surgery, machine learning systems can monitor vital signs and other data, alerting surgeons to any concerning changes instantly.
However, the integration of machine learning into surgical practices isn't without its challenges. There are concerns about the reliability of algorithms and the quality of data they are trained on. If the data is biased or incomplete, the outcomes could be detrimental. Surgeons must remain vigilant and not rely solely on these technologies. Instead, they should view machine learning as a powerful ally—one that complements their expertise rather than replaces it.
In summary, machine learning is transforming surgical decision-making by improving diagnostics, personalizing treatment, and providing real-time insights. As these technologies continue to evolve, they hold the promise of making surgery safer and more effective, ultimately leading to better patient outcomes. It's an exciting time for the field, and as we embrace these advancements, we must also consider the ethical implications and ensure that patient safety remains the top priority.

Ethical Considerations in AI Surgery
The integration of artificial intelligence (AI) into surgical practices is revolutionizing the field, but it also raises significant ethical considerations that cannot be overlooked. As we embrace these advanced technologies, we must grapple with questions surrounding data privacy, accountability, and the potential for bias in AI algorithms. These issues are not merely academic; they have real implications for patient safety and trust in the healthcare system.
One of the foremost ethical concerns is data privacy. AI systems rely on vast amounts of data to learn and make decisions. This data often includes sensitive patient information. The question arises: how is this data collected, stored, and used? Patients must be assured that their personal health information is protected and that AI systems adhere to strict data privacy regulations. Furthermore, there's the risk of data breaches, which can lead to unauthorized access to personal information, potentially harming patients and eroding their trust in healthcare providers.
Another critical aspect is accountability. When an AI system makes a mistake during a surgical procedure, who is held responsible? Is it the surgeon, the hospital, or the developers of the AI technology? This ambiguity can create significant legal and ethical dilemmas. As AI becomes more autonomous, establishing clear lines of accountability is essential to ensure that patients are protected and that healthcare providers are held to high standards of care.
Moreover, the potential for bias in AI algorithms poses a serious ethical challenge. AI systems are only as good as the data they are trained on. If the training data is biased, the AI's decisions will reflect those biases, leading to inequitable treatment outcomes. For instance, if an AI system is primarily trained on data from a specific demographic, it may not perform as effectively for patients outside that demographic. This could exacerbate existing health disparities and undermine the principle of equitable care.
To address these ethical concerns, it is vital to implement robust guidelines and regulations governing the use of AI in surgery. Transparency is key; patients should be informed about how AI is being used in their care. This includes understanding the role of AI in diagnostics, treatment planning, and even the surgical procedure itself. Informed consent must extend beyond traditional parameters to encompass the implications of AI involvement.
Additionally, healthcare providers must engage in continuous education and training regarding the ethical use of AI technologies. This includes understanding the limitations of AI, recognizing potential biases, and being prepared to explain AI's role in patient care clearly and effectively. Only through a commitment to ethical practices can we harness the full potential of AI in surgery while safeguarding patient rights and well-being.
- What are the main ethical concerns regarding AI in surgery? The primary concerns include data privacy, accountability, and potential bias in AI algorithms.
- How can patients ensure their data is protected? Patients should inquire about the data privacy policies of their healthcare providers and how their information will be used and stored.
- Who is responsible if an AI system makes a mistake during surgery? Accountability is a complex issue, and it can fall on the surgeon, the healthcare institution, or the AI technology developers, depending on the situation.
- What can be done to prevent bias in AI systems? Ensuring diverse and representative training data and conducting regular audits of AI systems can help mitigate bias.

Patient Consent and AI
In the realm of AI-guided surgeries, the concept of patient consent takes on a new dimension. Traditionally, patients have been asked to consent to surgical procedures based on a clear understanding of the methods and risks involved. However, with the advent of artificial intelligence in surgical practices, the landscape is evolving rapidly. Patients now face the challenge of understanding not only the surgical procedure itself but also the role that AI technologies play in their treatment. This raises the question: how can we ensure that patients are fully informed and comfortable with these advanced technologies?
One critical aspect of obtaining informed consent is transparency. Patients should be made aware of how AI systems will be utilized during their surgery. For instance, if machine learning algorithms are involved in diagnostic processes or surgical planning, it’s essential to explain how these algorithms function and the benefits they may offer. This can help demystify AI for patients, allowing them to grasp its significance in enhancing their surgical outcomes.
Moreover, the consent process should include discussions about potential risks associated with AI technologies. While AI can significantly improve surgical precision, it is not infallible. Patients should understand that there are inherent risks, including the possibility of errors in data interpretation or algorithm bias that could influence surgical decisions. By openly addressing these concerns, healthcare providers can foster a sense of trust and collaboration between themselves and their patients.
To facilitate this understanding, healthcare professionals might consider using visual aids or simplified explanations when discussing AI technologies. For example, a patient information brochure could outline the role of AI in their surgery, including:
- What AI technologies are being used
- How these technologies enhance surgical outcomes
- Possible risks and limitations
- Patient rights and options regarding AI involvement
Additionally, it’s vital to create an environment where patients feel comfortable asking questions. Encouraging an open dialogue allows patients to voice their concerns and seek clarification, ensuring they are not just passively signing consent forms but actively participating in their healthcare decisions.
Ultimately, the goal of informed consent in AI-guided surgeries is to empower patients. By providing comprehensive information and fostering open communication, healthcare providers can help patients make informed choices about their treatment. This not only enhances the patient experience but also aligns with ethical standards in healthcare, ensuring that patients feel respected and valued as partners in their care.
As we navigate the complexities of AI in surgery, many questions arise. Here are some frequently asked questions regarding patient consent and AI:
| Question | Answer |
|---|---|
| What is AI-guided surgery? | AI-guided surgery utilizes artificial intelligence technologies to assist surgeons in making more accurate and efficient decisions during surgical procedures. |
| How does AI impact patient consent? | AI impacts patient consent by introducing new elements that patients need to understand, such as the role of AI in their surgical process and the associated risks. |
| Are there risks involved with AI in surgery? | Yes, while AI can enhance precision, there are risks such as potential algorithm bias or errors in data interpretation that patients should be aware of. |
| How can I prepare for discussions about AI in my surgery? | Patients should prepare by asking questions, seeking clarification on AI technologies involved, and understanding their rights regarding consent. |

Accountability and Liability Issues
As the integration of artificial intelligence (AI) into surgical practices continues to evolve, the questions surrounding accountability and liability become increasingly pertinent. Who is responsible when an AI-assisted surgery does not go as planned? Is it the surgeon, the hospital, or the developers of the AI technology? These questions are not just academic; they have real implications for patient safety and the legal landscape of healthcare.
One of the most pressing concerns is the legal accountability of healthcare professionals when AI technologies are employed. Traditionally, surgeons have been held accountable for the outcomes of their procedures. However, with AI systems making recommendations or even controlling surgical instruments, the lines of responsibility can become blurred. For instance, if a surgical error occurs due to a malfunction in an AI system, determining liability can be a complex process. Should the blame fall on the surgeon who relied on the AI, the hospital that implemented the technology, or the company that designed the software?
To address these issues, several legal frameworks are being proposed. These frameworks aim to clarify the responsibilities of each party involved in AI-assisted surgeries. For example, some suggest that hospitals should ensure that their staff are adequately trained in both the technology and its limitations. Others advocate for stricter regulations on AI development to ensure that these systems are robust and reliable before they are used in clinical settings.
Moreover, ethical considerations must also be taken into account. The use of AI in surgery raises questions about informed consent. Patients must understand how AI is being used in their procedures and the potential risks involved. Transparency is key; patients should be made aware of the role of AI in their treatment, which can help build trust and ensure that they are making informed decisions about their healthcare.
Furthermore, the potential for bias in AI algorithms can complicate accountability. If an AI system is trained on biased data, it may lead to unequal treatment outcomes for different patient populations. This raises ethical concerns about fairness and equality in healthcare, and it places additional responsibility on developers and healthcare providers to ensure that AI systems are designed and implemented in a way that promotes equity.
In summary, as we venture further into the realm of AI-guided surgeries, the issues of accountability and liability will require careful consideration and ongoing dialogue among healthcare professionals, legal experts, and ethicists. The future of surgical practices will not only depend on technological advancements but also on how we navigate these complex issues to ensure patient safety and uphold the standards of care.
- Who is liable if an AI-assisted surgery goes wrong?
Liability can fall on multiple parties, including the surgeon, the hospital, and the AI technology developers, depending on the circumstances. - What role does informed consent play in AI surgeries?
Patients must be informed about the use of AI in their procedures and understand the associated risks to make educated decisions. - How can bias in AI algorithms affect surgical outcomes?
Bias in AI can lead to unequal treatment outcomes, emphasizing the need for fairness in AI system design and implementation.
Frequently Asked Questions
- What is AI-guided surgery?
AI-guided surgery refers to the use of artificial intelligence technologies to assist surgeons in performing operations. By leveraging advanced algorithms and data analysis, AI can enhance surgical precision, improve decision-making, and ultimately lead to better patient outcomes.
- How has surgical technology evolved over the years?
Surgical technology has seen remarkable advancements, from traditional open surgeries to minimally invasive techniques. Key milestones include the introduction of laparoscopic procedures, robotic systems, and now, the integration of AI, which is revolutionizing how surgeries are performed.
- What are the benefits of robotic-assisted surgery?
Robotic-assisted surgery offers numerous advantages such as increased precision, reduced blood loss, and shorter recovery times. These systems allow surgeons to perform complex procedures with greater control and less trauma to the patient's body.
- What challenges do robotic surgeries face?
While robotic surgery has many benefits, it also comes with challenges like high costs, the need for specialized training, and potential technical issues during operations. These factors can limit accessibility and effectiveness in certain situations.
- How does machine learning improve surgical decision-making?
Machine learning algorithms analyze vast amounts of data to provide surgeons with insights during procedures. This technology can assist in diagnostics and treatment planning, helping to ensure that patients receive the most effective care possible.
- What ethical considerations are there in AI surgery?
AI surgery raises important ethical questions, including data privacy, accountability, and potential biases in algorithms. It's crucial for healthcare providers to address these concerns to maintain trust and ensure patient safety.
- How is patient consent handled in AI-guided surgeries?
Informed consent is vital in AI-guided surgeries. Patients must understand how AI will be used in their treatment and the potential risks involved. Transparency is key to ensuring that patients feel comfortable and informed about their surgical options.
- Who is accountable if something goes wrong during an AI-assisted surgery?
Accountability in AI-assisted surgeries can be complex. Healthcare providers must navigate legal and ethical responsibilities, ensuring that patient safety is prioritized while also addressing the implications of AI technology in their practices.