The Strength of AI in Cancer Diagnosis and Treatment
In recent years, the landscape of healthcare has been dramatically transformed by the advent of artificial intelligence (AI). This technology is not just a buzzword; it's a game-changer, especially in the field of oncology. Imagine a world where cancer is detected earlier, treatment plans are tailored specifically to individual patients, and outcomes are significantly improved. That's the promise of AI in cancer diagnosis and treatment. By leveraging vast amounts of data and sophisticated algorithms, AI is enhancing the way healthcare professionals approach cancer care, making it more precise and efficient. But what exactly does this entail? Let’s dive into the transformative role of AI in revolutionizing how we detect and treat cancer.
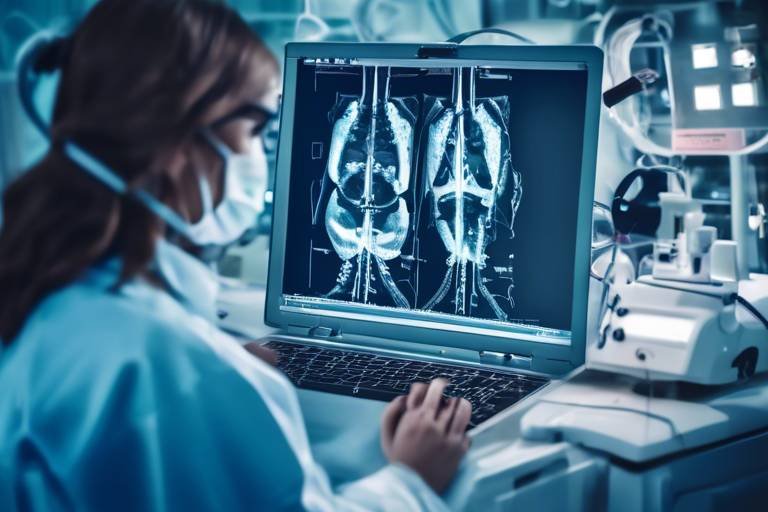
Early detection of cancer is crucial for effective treatment and improved survival rates. AI technologies are leading the charge in this area, offering tools that analyze medical images and patient data with incredible speed and accuracy. For instance, AI algorithms can sift through thousands of medical images to identify subtle patterns that may be indicative of cancer, patterns that the human eye might miss. This capability not only accelerates the diagnostic process but also enhances the accuracy of the results, leading to quicker interventions. The effectiveness of these AI-driven techniques is evident in various studies, showing a significant increase in early-stage cancer detection rates.
When it comes to diagnostic imaging, AI algorithms are proving to be invaluable. These advanced systems are being integrated into various imaging techniques such as X-rays, CT scans, and MRIs, allowing for more accurate interpretations of scans. What does this mean for patient care? It means that healthcare providers can make more informed decisions faster. For instance, an AI system might analyze a CT scan and highlight areas of concern, enabling radiologists to focus their attention where it’s needed most. The implications for patient care are profound, as more accurate diagnostics lead to timely and appropriate treatments.
Machine learning, a subset of AI, is making waves in the field of radiology. By training on vast datasets of medical images, these models learn to identify cancerous lesions with remarkable precision. Imagine having a virtual assistant that never tires and constantly learns from new data – that's what machine learning brings to the table. These models enhance the efficiency and accuracy of radiologists, allowing them to spend more time on patient care rather than on tedious image analysis. As a result, the diagnostic process becomes not only faster but also more reliable.
Real-world case studies provide compelling evidence of the successful implementation of machine learning in radiology. For example, a recent study demonstrated that AI-assisted imaging led to a 30% increase in the detection rates of early-stage lung cancer among radiologists. This improvement also translated into greater diagnostic confidence, as healthcare professionals felt more assured in their evaluations when supported by AI technology. These case studies highlight the tangible benefits of AI, showcasing how it can lead to better patient outcomes.
Despite its many advantages, the integration of machine learning into radiology does not come without challenges. Issues such as data privacy concerns and the necessity for ongoing training of healthcare personnel are significant hurdles that must be addressed. Ensuring that patient data is protected while also providing healthcare workers with the tools and knowledge they need to utilize AI effectively is crucial for the successful adoption of these technologies.
AI is also making significant strides in the field of pathology, where it assists in analyzing tissue samples. By employing sophisticated algorithms, AI enhances diagnostic precision, enabling pathologists to evaluate samples more accurately. This technological support is particularly beneficial in identifying cancerous cells and determining the best course of action for treatment. With AI, pathologists can process and interpret complex data sets much faster, leading to quicker diagnoses and improved patient management.
The concept of personalized medicine is becoming a reality thanks to AI. By analyzing a patient's unique data, including genetic information and treatment history, AI can predict how a patient will respond to specific treatments. This tailored approach not only enhances the efficacy of cancer therapies but also minimizes potential side effects. Imagine being able to choose a treatment plan that is customized just for you, based on your individual characteristics. This is the future of cancer treatment, and AI is at the forefront of making it happen.
Predictive analytics powered by AI allows oncologists to forecast treatment efficacy based on individual patient profiles. By utilizing historical data and advanced algorithms, these predictive models can provide insights into which treatments are likely to be the most effective for a particular patient. This methodology not only streamlines the decision-making process but also empowers patients by giving them a clearer understanding of their treatment options.
AI technologies are also revolutionizing drug discovery processes, significantly accelerating the identification of potential candidates for cancer treatment. Traditional drug development can take years, but with AI, researchers can analyze vast datasets to uncover new therapeutic targets and streamline the development of innovative therapies. This efficiency not only shortens research timelines but also holds the promise of delivering effective treatments to patients sooner than ever before.
- What is the role of AI in cancer diagnosis? AI assists in analyzing medical images and patient data to improve early detection and accuracy of cancer diagnoses.
- How does AI improve treatment plans? AI analyzes individual patient data to create personalized treatment plans that predict the best therapeutic responses.
- Are there challenges in implementing AI in healthcare? Yes, challenges include data privacy concerns and the need for continuous training of healthcare professionals.
- Can AI help in drug discovery? Absolutely! AI accelerates the drug discovery process by analyzing large datasets to identify potential treatment candidates more efficiently.

The Role of AI in Early Detection
Artificial Intelligence (AI) is rapidly transforming the landscape of cancer detection, making significant strides in the early identification of malignancies. Imagine a world where a simple scan can reveal the presence of cancer long before symptoms arise; that's the power of AI in action. By leveraging advanced algorithms and machine learning techniques, AI systems can analyze vast amounts of medical data and images with remarkable speed and accuracy. This capability not only accelerates the diagnostic process but also enhances the overall effectiveness of patient care.
One of the most significant advantages of AI in early detection lies in its ability to process and interpret medical imaging. Traditional methods often rely heavily on the expertise of radiologists, which can lead to variability in diagnosis. However, AI tools are designed to recognize patterns and anomalies in imaging scans, such as X-rays, MRIs, and CT scans, with a level of precision that often surpasses human capabilities. For instance, AI can detect minute changes in tissue density or structure that may indicate the presence of a tumor, often identifying conditions at stages where they are most treatable.
To illustrate the effectiveness of AI in early detection, consider the following key techniques:
- Deep Learning: This subset of machine learning uses neural networks to analyze images and has shown exceptional promise in identifying breast cancer in mammograms.
- Natural Language Processing (NLP): NLP algorithms can sift through unstructured data in medical records to uncover critical information that could indicate early signs of cancer.
- Predictive Analytics: By analyzing patient history and genetic data, AI can predict an individual's risk of developing certain types of cancer, enabling proactive monitoring and intervention.
The results of these AI applications are nothing short of revolutionary. Studies have demonstrated that AI can reduce false positives and negatives, leading to a more reliable diagnostic process. For example, a recent study revealed that AI-assisted mammography improved breast cancer detection rates by over 10%, significantly enhancing early diagnosis and increasing the likelihood of successful treatment outcomes.
However, the integration of AI into early detection is not without its challenges. Issues such as data privacy, the need for large datasets for training AI models, and the requirement for healthcare professionals to adapt to new technologies remain critical hurdles. Nevertheless, as AI continues to evolve, its role in early cancer detection is expected to expand, paving the way for a future where early diagnosis becomes the norm rather than the exception.
In summary, AI's capabilities in early cancer detection are reshaping the medical field. With its ability to analyze complex data quickly and accurately, AI not only enhances diagnostic efficiency but also significantly improves patient outcomes. As we look ahead, the potential for AI to save lives through earlier detection is immense, making it an invaluable tool in the fight against cancer.

AI Algorithms in Diagnostic Imaging
In the realm of modern medicine, AI algorithms are proving to be game-changers in diagnostic imaging. They are not just tools; they are revolutionizing the way we interpret medical scans, enhancing accuracy and efficiency in detecting diseases like cancer. Imagine having a virtual assistant that never tires, tirelessly analyzing images and pointing out anomalies that a human eye might miss. That's the power of AI in diagnostic imaging!
AI algorithms are designed to process vast amounts of imaging data, utilizing techniques such as deep learning and neural networks. These algorithms learn from thousands of annotated images, developing the ability to recognize patterns associated with various types of cancer. For instance, in mammography, AI can identify subtle signs of breast cancer that may not be evident to radiologists, leading to earlier detection and better outcomes for patients.
One of the most exciting aspects of AI in diagnostic imaging is its ability to integrate with various imaging modalities. Whether it’s CT scans, MRI, or X-rays, AI algorithms can enhance the interpretation of these images. For example, in a recent study, an AI system was able to analyze CT scans of lung cancer patients with a remarkable accuracy rate, surpassing traditional methods. This not only saves time but also aids in making more informed decisions regarding patient treatment.
To give you a clearer picture of how AI is transforming diagnostic imaging, consider the following table that highlights the key imaging techniques enhanced by AI:
| Imaging Technique | AI Enhancement | Benefits |
|---|---|---|
| CT Scans | Automated lesion detection | Faster diagnosis, improved accuracy |
| MRI | Image segmentation | Better visualization of tumors |
| Mammography | Pattern recognition | Early detection of breast cancer |
| X-rays | Anomaly detection | Reduced false positives |
However, the implementation of AI algorithms in diagnostic imaging is not without its challenges. One major concern is the interpretability of AI decisions. While these algorithms can provide accurate results, understanding how they arrive at their conclusions can be complex. This creates a need for collaboration between AI systems and human radiologists to ensure that the insights provided by AI are not only accurate but also understandable.
Moreover, data privacy and security are paramount. As AI systems require access to vast amounts of patient data to learn and improve, ensuring that this data is handled securely is crucial. The healthcare industry must navigate these challenges carefully to harness the full potential of AI.
In conclusion, AI algorithms are paving the way for a new era in diagnostic imaging. By enhancing the accuracy and efficiency of image analysis, they are not only improving patient outcomes but also empowering healthcare professionals. As we continue to explore the capabilities of AI, the future of cancer diagnosis looks brighter than ever.

Machine Learning in Radiology
Machine learning is transforming the field of radiology, acting as a powerful ally for radiologists in the quest for precise cancer diagnosis. Imagine having a tool that not only helps in identifying cancerous lesions but also learns from every scan it analyzes. This is precisely what machine learning models do—they continuously improve their accuracy by processing vast amounts of imaging data. By utilizing algorithms that can detect patterns invisible to the human eye, these models enhance the efficiency and effectiveness of radiological assessments.
One of the most notable aspects of machine learning in radiology is its ability to analyze medical images such as X-rays, CT scans, and MRIs. For instance, when presented with thousands of images labeled with various conditions, these algorithms can learn to identify subtle differences between benign and malignant tissues. As a result, they can assist radiologists in making quicker and more accurate diagnoses. This is not just a theoretical advantage; studies have shown that machine learning can improve diagnostic accuracy by up to 20% in certain cases.
Moreover, the training of these models involves a process known as supervised learning, where the algorithm is fed a large dataset of images along with their corresponding diagnoses. Over time, the model learns to recognize the features that distinguish one condition from another. This training phase is crucial, as the quality and diversity of the data used can significantly impact the model's performance. In practice, this means that the more varied the dataset—encompassing different demographics, imaging techniques, and cancer types—the better the algorithm can perform across a broader spectrum of cases.
However, it's essential to note that while machine learning can significantly enhance diagnostic capabilities, it does not replace the human touch that radiologists bring to the table. Instead, it acts as a supportive tool, allowing radiologists to focus on more complex cases and make informed decisions based on the insights provided by the algorithms. This collaboration between human expertise and machine intelligence is paving the way for a new era in cancer diagnosis.
In addition to improving detection rates, machine learning can also reduce the workload of radiologists. With the ability to pre-screen images and flag potential issues, radiologists can prioritize cases that require immediate attention, thus streamlining the entire diagnostic process. This efficiency can lead to faster treatment decisions, ultimately benefiting patients who are often in urgent need of care.
As we look to the future, the integration of machine learning in radiology is expected to expand. With advancements in technology and the continuous influx of data, these algorithms will become even more sophisticated. They will not only aid in diagnosis but could also contribute to predictive analytics, helping to forecast patient outcomes based on imaging findings. The potential is immense, and the journey has only just begun.
- What is machine learning in radiology? Machine learning in radiology involves the use of algorithms to analyze medical images, helping radiologists detect and diagnose conditions more accurately and efficiently.
- How does machine learning improve cancer detection? By identifying patterns in imaging data that may be missed by human eyes, machine learning can enhance the accuracy of cancer diagnoses and reduce false positives.
- Is machine learning going to replace radiologists? No, machine learning is designed to assist radiologists, not replace them. It enhances their capabilities and allows them to focus on more complex cases.
- What types of imaging can benefit from machine learning? Machine learning can be applied to various imaging types, including X-rays, CT scans, MRIs, and even ultrasound images.

Case Studies in Radiology
In the rapidly evolving field of radiology, the integration of artificial intelligence (AI) has led to remarkable advancements, particularly in cancer detection. Numerous case studies have emerged, showcasing how AI technologies are not just theoretical concepts but practical tools that enhance diagnostic accuracy and efficiency. One notable example comes from a study conducted at a leading cancer center, where AI algorithms were implemented to analyze mammography images. The results were astonishing; the AI system was able to detect breast cancer with a sensitivity rate of over 94%, significantly higher than the traditional methods that hovered around 80%.
Another compelling case study involved the use of deep learning algorithms in the detection of lung cancer from CT scans. Researchers found that the AI model could identify malignant nodules with a specificity of 90%, which not only reduced false positives but also alleviated the stress and anxiety often experienced by patients awaiting diagnosis. In this scenario, the AI acted almost like a seasoned detective, sifting through mountains of data to uncover hidden clues that even the most experienced radiologists might overlook.
Moreover, a collaborative study between several hospitals demonstrated the impact of AI on workflow efficiency. By integrating AI into the radiology department, the average time taken to interpret scans was reduced by 30%. This translated into quicker diagnoses for patients, allowing for earlier treatment interventions. The radiologists involved reported that they could focus on more complex cases while the AI handled routine screenings, thereby enhancing overall productivity.
To illustrate the effectiveness of these AI systems, here’s a summary table of key findings from various studies:
| Study | Technology Used | Outcome | Sensitivity/Specificity |
|---|---|---|---|
| Mammography Study | AI Algorithm | Improved detection rates | 94% Sensitivity |
| Lung Cancer Detection | Deep Learning | Reduced false positives | 90% Specificity |
| Workflow Efficiency | AI Integration | Faster scan interpretation | 30% Time Reduction |
These case studies not only highlight the potential of AI in enhancing diagnostic accuracy but also underscore the importance of ongoing research and development in this area. As technology continues to advance, it is crucial for healthcare professionals to stay informed about the latest AI tools and their applications in radiology. The future of cancer detection looks promising, and with AI by our side, we are one step closer to achieving earlier diagnoses and better patient outcomes.
- What is the role of AI in cancer diagnosis? AI assists in analyzing medical images, improving detection rates, and enabling quicker diagnoses.
- How does AI improve radiology efficiency? AI algorithms can process and interpret scans faster than human radiologists, allowing them to focus on more complex cases.
- Are there any challenges in implementing AI in radiology? Yes, challenges include data privacy concerns and the need for continuous training of healthcare personnel.
- What is the future of AI in cancer treatment? AI is expected to play a significant role in personalized treatment plans and drug discovery, leading to improved patient outcomes.

Challenges in Implementation
While the integration of AI in cancer diagnosis and treatment presents remarkable opportunities, it also comes with a set of significant challenges that need to be addressed. One of the primary hurdles is data privacy concerns. With the vast amounts of sensitive patient data required to train AI algorithms, ensuring that this information is protected from breaches is critical. Healthcare providers must navigate complex regulations, such as HIPAA in the United States, to maintain patient confidentiality while leveraging AI technologies.
Another challenge is the need for ongoing training of healthcare personnel. As AI systems evolve, medical professionals must continuously update their skills to effectively use these advanced tools. This includes understanding how to interpret AI-generated results and integrating these insights into their clinical decision-making processes. Without proper training, the potential benefits of AI can be undermined, leading to misinterpretations that could adversely affect patient care.
Moreover, there is often a resistance to change within the medical community. Many healthcare professionals may feel apprehensive about relying on AI technologies, fearing that they could replace human expertise. This perception can create a barrier to the adoption of these innovative tools, even when they have been shown to enhance diagnostic accuracy and efficiency. Building trust in AI systems is essential, and this can be achieved through transparent communication and demonstrating the value of AI in improving patient outcomes.
Additionally, the quality of data used to train AI algorithms is paramount. If the data is biased or not representative of diverse populations, the AI systems may yield inaccurate results, leading to disparities in care. Ensuring that AI models are trained on high-quality, diverse datasets is crucial to mitigate these risks. This involves collaboration between data scientists, clinicians, and ethicists to create robust datasets that reflect the variability found in real-world patient populations.
Lastly, the cost of implementation cannot be overlooked. Developing and integrating AI technologies into existing healthcare infrastructures requires significant financial investment. This can be a daunting prospect for many healthcare organizations, especially smaller practices or those in underserved areas. To overcome this barrier, stakeholders must explore funding opportunities and partnerships that can support the sustainable integration of AI in cancer care.
- What are the main challenges of implementing AI in cancer treatment?
Key challenges include data privacy concerns, the need for ongoing training of healthcare personnel, resistance to change among medical professionals, the quality of data used for training AI systems, and the cost of implementation.
- How can healthcare professionals overcome resistance to AI?
Building trust in AI systems through transparent communication, demonstrating their effectiveness, and providing adequate training can help alleviate concerns among healthcare professionals.
- What role does data quality play in AI implementation?
The quality of data is crucial as biased or unrepresentative data can lead to inaccurate AI results, potentially resulting in disparities in patient care.
- Are there funding options available for AI implementation in healthcare?
Yes, exploring partnerships, grants, and other funding opportunities can help healthcare organizations manage the costs associated with AI integration.

AI in Pathology
Artificial Intelligence (AI) is making significant strides in the field of pathology, where it plays a pivotal role in enhancing the analysis of tissue samples. Imagine a world where pathologists, the unsung heroes of cancer diagnosis, are equipped with intelligent systems that can assist them in their evaluations. This is not just a futuristic dream; it’s becoming a reality as AI technologies are increasingly integrated into pathology workflows. By employing advanced algorithms and machine learning techniques, AI can analyze vast amounts of data from tissue samples much faster than a human ever could, leading to more accurate diagnoses.
One of the most exciting aspects of AI in pathology is its ability to improve diagnostic precision. Traditional pathology relies heavily on the expertise of pathologists who examine tissue samples under a microscope. While they are incredibly skilled, the process is inherently subjective and can be influenced by fatigue or varying levels of experience. AI, on the other hand, can provide a consistent and objective analysis, reducing the likelihood of human error. For instance, AI systems can highlight areas of concern in a tissue sample, allowing pathologists to focus their attention where it is needed most. This collaboration between human expertise and AI technology not only speeds up the diagnostic process but also enhances the overall quality of care provided to patients.
Moreover, AI can assist in identifying subtle patterns in the data that may not be immediately visible to the human eye. Using techniques such as image recognition, AI can analyze histopathological images and identify cancerous cells with remarkable accuracy. This capability is particularly crucial in cases where early detection is vital for successful treatment outcomes. In fact, studies have shown that AI can match or even exceed the diagnostic accuracy of experienced pathologists in certain scenarios.
However, the integration of AI into pathology is not without its challenges. One significant concern is the need for high-quality data to train these AI systems. Pathology relies on large datasets of annotated tissue samples to teach AI models how to recognize different types of cancer. Without sufficient data, the effectiveness of AI can be compromised. Additionally, there is an ongoing debate about the ethical implications of relying on AI for medical diagnoses. Questions surrounding data privacy, the potential for bias in AI algorithms, and the need for transparency in AI decision-making processes are all critical considerations that must be addressed as we move forward.
Despite these challenges, the future of AI in pathology looks promising. As technology continues to advance and more data becomes available, we can expect to see even more sophisticated AI systems that can assist pathologists in their critical work. The potential benefits are immense, including faster diagnoses, improved patient outcomes, and a more efficient healthcare system overall. In this rapidly evolving landscape, it’s essential for healthcare professionals to stay informed about the latest developments in AI and its applications in pathology.
- What is the role of AI in pathology? AI assists pathologists by analyzing tissue samples more quickly and accurately, enhancing diagnostic precision.
- How does AI improve diagnostic accuracy? AI can identify subtle patterns in tissue samples that may be missed by human eyes, leading to more reliable diagnoses.
- What are the challenges of implementing AI in pathology? Key challenges include the need for high-quality training data, ethical considerations regarding data privacy, and potential biases in AI algorithms.
- What does the future hold for AI in pathology? The future looks promising, with advancements expected to lead to more sophisticated AI systems that improve patient outcomes and streamline healthcare processes.

Personalized Treatment Plans with AI
In the realm of cancer treatment, the phrase “one size fits all” is becoming increasingly outdated. Thanks to the incredible advancements in artificial intelligence (AI), we are venturing into an era where personalized treatment plans are not just a possibility but a reality. Imagine a world where your treatment is tailored specifically to your unique genetic makeup and medical history—sounds like something out of a science fiction novel, right? But it's happening now!
AI is revolutionizing oncology by analyzing vast amounts of patient data to create individualized treatment strategies. By leveraging predictive analytics, AI can forecast how a patient might respond to various treatments based on their specific biological markers and other relevant factors. This means that oncologists can move away from generalized treatment protocols and instead focus on what works best for each patient. It’s like having a personal coach for your health—one that knows exactly how to maximize your chances of recovery.
To illustrate this, let’s dive into some of the methodologies that AI employs to create these personalized treatment plans:
- Data Integration: AI systems aggregate data from multiple sources, including genomic data, clinical records, and even lifestyle factors. This holistic view allows for a more comprehensive understanding of the patient’s condition.
- Machine Learning Algorithms: These algorithms analyze patterns in the data, identifying which treatments have been effective for similar patients in the past. It’s like having a vast library of treatment outcomes at your fingertips!
- Real-Time Monitoring: AI can continuously assess a patient's response to treatment, making adjustments in real-time. This dynamic approach ensures that any potential issues are addressed promptly, leading to better outcomes.
Moreover, the impact of AI in creating personalized treatment plans extends beyond just the initial diagnosis. It plays a crucial role in the ongoing management of cancer care. For instance, as new research emerges or as a patient’s condition evolves, AI can help oncologists adapt treatment strategies to ensure maximum efficacy. This adaptability is essential in the ever-changing landscape of cancer therapy, where new information can dramatically shift the course of treatment.
Another exciting aspect of AI in personalized treatment is its potential in drug discovery. Traditional drug development can take years, but AI accelerates this process by identifying promising compounds and predicting their effectiveness against specific cancer types. This not only shortens the timeline for bringing new therapies to market but also enhances the chances of finding the right drug for the right patient.
In summary, the integration of AI into personalized treatment plans is a game-changer in the fight against cancer. By harnessing the power of data and advanced algorithms, healthcare providers can offer tailored treatments that improve patient outcomes and enhance the quality of life for those battling this disease. The future of oncology is bright, and AI is leading the charge!
Q: How does AI personalize cancer treatment?
AI personalizes cancer treatment by analyzing patient data, including genetic information, to determine the most effective therapies tailored to individual needs.
Q: What role does predictive analytics play in oncology?
Predictive analytics helps oncologists anticipate how a patient will respond to specific treatments, allowing for more informed and personalized care decisions.
Q: Can AI help in drug discovery for cancer treatments?
Yes, AI significantly speeds up drug discovery by identifying potential drug candidates and predicting their effectiveness, thereby reducing the time it takes to bring new therapies to patients.
Q: Are there any risks associated with AI in cancer treatment?
While AI offers numerous benefits, challenges such as data privacy concerns and the need for continuous training of healthcare professionals must be addressed to ensure safe and effective use.

Predictive Analytics in Oncology
Predictive analytics is emerging as a game-changer in the field of oncology, revolutionizing how oncologists approach cancer treatment. By leveraging vast amounts of patient data, including genetic information, treatment histories, and lifestyle factors, predictive analytics enables healthcare professionals to forecast treatment outcomes with remarkable accuracy. Imagine being able to predict how a specific patient will respond to a particular treatment before it's even administered—this is the promise of predictive analytics in oncology. It’s like having a crystal ball that allows doctors to tailor treatments to the individual, enhancing the likelihood of successful outcomes.
At the heart of this transformation are sophisticated algorithms that analyze complex datasets. These algorithms identify patterns and correlations that may not be immediately apparent to human clinicians. For instance, they can evaluate the effectiveness of various therapies based on historical data from similar patients. This capability not only streamlines the decision-making process but also empowers oncologists to make informed choices that align with each patient's unique circumstances.
One of the most significant aspects of predictive analytics is its role in stratifying patients into different risk categories. By assessing factors such as tumor type, genetic markers, and response to previous treatments, oncologists can categorize patients into groups that may respond similarly to specific therapies. This stratification helps in designing personalized treatment plans that are more likely to yield positive results. For example, a patient with a specific genetic mutation may be directed toward targeted therapies that have proven effective for others with the same mutation, while another patient may be advised to consider alternative treatments based on their unique profile.
Moreover, predictive analytics can enhance clinical trials by identifying suitable candidates more efficiently. By analyzing patient data, researchers can pinpoint individuals who are most likely to benefit from experimental treatments, thus optimizing the trial process. This not only accelerates the pace of research but also increases the chances of finding effective therapies for various cancer types.
In summary, predictive analytics in oncology is not just about crunching numbers; it's about transforming patient care. By harnessing the power of data, oncologists can make more accurate predictions, leading to personalized treatment plans that improve outcomes and enhance the overall patient experience. As this field continues to evolve, we can expect even greater advancements that will further refine and redefine cancer treatment strategies.
- What is predictive analytics in oncology?
Predictive analytics in oncology refers to the use of data analysis techniques to forecast treatment outcomes and personalize cancer treatment plans.
- How does predictive analytics improve cancer treatment?
It allows oncologists to tailor treatments based on individual patient data, enhancing the likelihood of successful outcomes.
- Can predictive analytics be used in clinical trials?
Yes, it helps identify suitable candidates for clinical trials, optimizing the research process and improving the chances of finding effective therapies.

AI and Drug Discovery
In recent years, the intersection of artificial intelligence (AI) and drug discovery has emerged as a groundbreaking frontier in the fight against cancer. Traditionally, the process of discovering new drugs has been a lengthy and costly endeavor, often taking over a decade and billions of dollars to bring a single drug to market. However, with the advent of AI technologies, this landscape is changing rapidly. AI algorithms can analyze vast datasets, identify patterns, and predict how different compounds will interact with cancer cells, effectively streamlining the entire drug discovery process.
One of the most exciting aspects of AI in drug discovery is its ability to accelerate the identification of potential drug candidates. By utilizing machine learning techniques, researchers can sift through millions of chemical compounds and biological data points in a fraction of the time it would take a human researcher. This not only speeds up the discovery process but also increases the likelihood of finding effective treatments. For instance, AI can help in:
- Identifying new drug candidates: AI can predict which compounds are most likely to be effective against specific types of cancer.
- Optimizing existing drugs: AI can analyze data to suggest modifications to existing drugs, enhancing their efficacy or reducing side effects.
- Personalizing treatments: By analyzing genetic data, AI can help tailor drug therapies to individual patients, improving outcomes.
Furthermore, AI's role in drug discovery extends to predictive modeling. By using historical data on drug interactions and patient outcomes, AI models can forecast how new drugs will perform in clinical settings. This predictive capability is crucial, as it allows researchers to prioritize the most promising candidates for further development, saving both time and resources. For example, a study published in a leading medical journal demonstrated that AI-driven models could predict the success rate of new cancer therapies with an accuracy of over 85%, a significant improvement over traditional methods.
However, despite these advancements, the integration of AI into drug discovery is not without challenges. Issues such as data quality, regulatory hurdles, and the need for interdisciplinary collaboration remain significant barriers. Researchers must ensure that the data used to train AI models is comprehensive and representative of diverse populations to avoid biases that could affect treatment efficacy. Moreover, regulatory bodies are still catching up with the rapid pace of AI development, necessitating clear guidelines to ensure the safe and effective use of AI in drug discovery.
To illustrate the impact of AI in drug discovery, let's consider a few notable case studies:
| Case Study | AI Technology Used | Outcome |
|---|---|---|
| Atomwise | Deep Learning | Identified potential compounds for Ebola treatment |
| BenevolentAI | Machine Learning | Developed a new treatment for ALS |
| Insilico Medicine | Generative Adversarial Networks | Discovered a new drug candidate for fibrosis |
As we look to the future, the potential of AI in drug discovery is enormous. With ongoing advancements in technology and an increasing understanding of cancer biology, we can expect to see even more innovative therapies emerging from this collaboration. The synergy between AI and drug discovery not only holds the promise of faster and more effective treatments but also paves the way for a new era of personalized medicine.
Q: How does AI improve the drug discovery process?
A: AI enhances drug discovery by analyzing large datasets to identify potential drug candidates, predict their efficacy, and optimize existing therapies, significantly reducing the time and cost of bringing new drugs to market.
Q: What are the main challenges in using AI for drug discovery?
A: Key challenges include ensuring data quality, addressing regulatory hurdles, and fostering interdisciplinary collaboration to effectively integrate AI technologies into existing drug development processes.
Q: Can AI personalize cancer treatments?
A: Yes, AI can analyze genetic and clinical data to tailor drug therapies to individual patients, thereby improving treatment outcomes and minimizing side effects.
Frequently Asked Questions
- What is the role of AI in early cancer detection?
AI plays a transformative role in early cancer detection by analyzing medical images and patient data more efficiently than traditional methods. This leads to quicker diagnoses, allowing for timely interventions and improved patient outcomes. By leveraging advanced algorithms, AI can identify subtle patterns in scans that may be missed by the human eye.
- How does AI enhance diagnostic imaging?
AI enhances diagnostic imaging by integrating advanced algorithms that improve the accuracy of scan interpretations. Techniques such as deep learning enable AI to process large datasets, allowing for more precise detection of abnormalities in imaging modalities like MRI, CT scans, and X-rays. This not only aids radiologists but also significantly boosts diagnostic confidence.
- What challenges are associated with implementing AI in radiology?
Despite its potential, implementing AI in radiology faces several challenges. Data privacy concerns are paramount, as sensitive patient information must be handled with care. Additionally, the continuous training of healthcare personnel is necessary to keep pace with evolving AI technologies, ensuring they can effectively interpret AI-assisted results.
- How does AI contribute to personalized cancer treatment?
AI contributes to personalized cancer treatment by analyzing individual patient data to predict treatment responses. By utilizing predictive analytics, oncologists can tailor treatment plans that are more effective for each patient, thereby improving outcomes. This approach considers genetic makeup, previous treatment responses, and other critical factors.
- What is the significance of predictive analytics in oncology?
Predictive analytics in oncology is significant because it allows healthcare providers to forecast treatment efficacy based on detailed patient profiles. This method helps in selecting the most suitable therapies, reducing trial-and-error approaches, and ultimately leading to better management of cancer care.
- How is AI changing the landscape of drug discovery for cancer treatments?
AI is revolutionizing drug discovery for cancer treatments by streamlining the identification of potential drug candidates. By analyzing vast amounts of data, AI can predict which compounds are likely to be effective, significantly cutting down research timelines. This innovation accelerates the development of new therapies, bringing hope to patients more quickly.