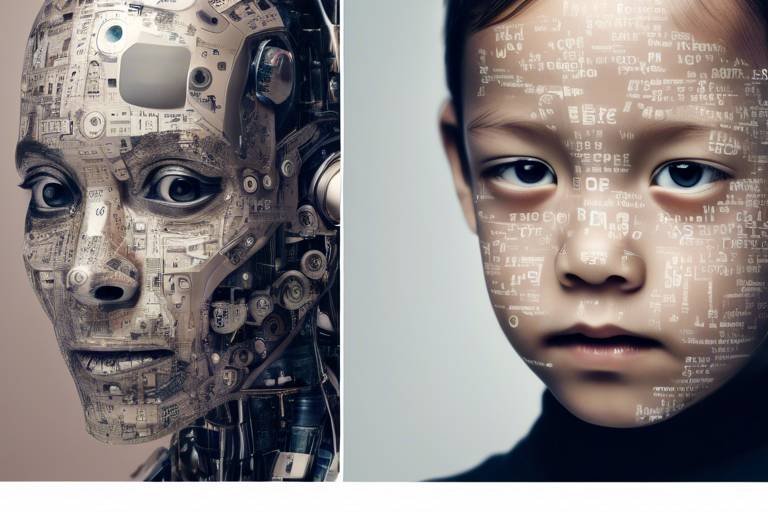
The Future of Healthcare with Artificial Intelligence and Robotics
In today's fast-paced world, the intersection of artificial intelligence (AI) and robotics is reshaping the landscape of healthcare as we know it. Imagine walking into a hospital where machines not only assist doctors but also enhance the accuracy of diagnoses, streamline surgical procedures, and monitor patients in real-time. This isn't science fiction; it's happening right now. The integration of these advanced technologies is not just a trend; it’s a revolution that promises to improve patient care significantly and optimize healthcare processes.
As we delve into the future, we find ourselves standing on the brink of what could be the most significant transformation in medical history. With AI algorithms capable of analyzing vast amounts of data and robotic systems that can perform intricate surgeries, the potential for better health outcomes is enormous. But what does this mean for healthcare professionals and patients alike? Are we ready to embrace this change, or are there challenges that we still need to address?
The benefits of incorporating AI and robotics into healthcare are multifaceted. For instance, AI can assist in diagnosing diseases at a much faster rate than traditional methods, allowing for timely interventions. Robotic systems can perform surgeries with precision that far exceeds human capabilities, leading to quicker recovery times and less post-operative pain for patients. However, with these advancements come questions about ethics, data privacy, and the potential for bias in AI algorithms.
Moreover, as we explore the future of healthcare, we must consider the implications of these technologies on healthcare professionals. Will they be replaced, or will they find new roles in this technologically advanced environment? While some fear that robots could take over jobs, the reality is that they are more likely to serve as powerful tools that augment the capabilities of healthcare workers. This partnership could lead to more efficient workflows and allow healthcare professionals to focus on what they do best: caring for patients.
In the upcoming sections, we will dive deeper into specific areas where AI and robotics are making a significant impact, from diagnostics to surgical procedures and patient monitoring. We will also discuss the ethical considerations that arise with these technologies, ensuring that we approach this exciting future with a comprehensive understanding of both the benefits and the challenges. Are you ready to explore how AI and robotics are transforming healthcare? Let’s dive in!
- What are the main benefits of AI in healthcare?
AI enhances diagnostics, streamlines processes, and improves patient outcomes by analyzing large datasets quickly. - How does robotic surgery differ from traditional surgery?
Robotic surgery offers greater precision, minimally invasive techniques, and reduced recovery times compared to traditional methods. - What ethical concerns are associated with AI in healthcare?
Concerns include data privacy, the potential for bias in algorithms, and the implications of AI on patient consent and decision-making. - Will healthcare professionals lose their jobs to robots?
While some fear job loss, robots are more likely to serve as tools that augment healthcare professionals' capabilities rather than replace them.

AI in Diagnostics
Artificial intelligence is not just a buzzword; it’s a game-changer in the field of diagnostics. Imagine a world where diseases are detected at their earliest stages, often before symptoms even appear. With AI, this is becoming a reality. By leveraging sophisticated algorithms and vast amounts of medical data, AI systems can analyze patterns that would be nearly impossible for humans to discern. This capability is transforming how we approach disease detection and patient diagnosis, leading to more timely and accurate results.
One of the most significant advantages of AI in diagnostics is speed. Traditional diagnostic methods often require multiple tests and lengthy waiting periods for results. In contrast, AI can process information in a fraction of the time, providing healthcare professionals with insights that can lead to immediate action. For instance, AI-powered imaging tools can analyze X-rays, MRIs, and CT scans in real-time, highlighting abnormalities that may indicate conditions such as cancer or fractures. This rapid analysis not only saves time but can also be crucial in emergency situations where every second counts.
Moreover, AI's ability to learn from vast datasets means that it continuously improves over time. As more data is fed into these systems, their accuracy and efficiency increase. This is particularly beneficial in fields like oncology, where early detection can significantly impact treatment outcomes. AI can help identify subtle changes in imaging results that may signal the onset of cancer, allowing for earlier interventions and potentially saving lives.
However, the integration of AI in diagnostics is not without its challenges. While the technology holds immense potential, it also raises questions about reliability and accountability. For example, if an AI system misdiagnoses a condition, who is responsible? Is it the healthcare provider who relied on the AI's recommendation, or the developers of the AI software? These are critical issues that the medical community must address as AI becomes more prevalent.
Despite these challenges, the potential benefits of AI in diagnostics far outweigh the drawbacks. A recent study showed that AI systems could outperform human radiologists in certain diagnostic tasks, achieving accuracy rates of over 95%. This impressive statistic underscores the importance of integrating AI into diagnostic processes. As we move forward, collaboration between AI developers, healthcare providers, and regulatory bodies will be essential to ensure that these technologies are used effectively and ethically.
In summary, AI is revolutionizing diagnostics by enhancing speed, accuracy, and learning capabilities. As we embrace this technology, we must also remain vigilant about the ethical considerations and strive for a future where AI and human expertise work hand in hand to improve patient outcomes.

Robotic Surgery
Robotic surgery is not just a trend; it's a revolution in the way surgical procedures are performed. Imagine a surgeon, not just using their hands, but also having the assistance of a highly advanced robotic system that enhances their precision and control during operations. This fusion of human expertise and robotic technology is changing the landscape of surgery, making it safer, more efficient, and less invasive for patients. The benefits of robotic-assisted surgeries are numerous, including significantly reduced recovery times, minimal scarring, and improved surgical outcomes. With these systems, the surgeon can perform complex procedures with enhanced dexterity, as if they were using their own hands, but with the added advantage of robotic precision.
One of the standout features of robotic surgery is its ability to perform minimally invasive procedures. Traditional surgeries often require large incisions, which can lead to longer recovery periods and increased pain for patients. In contrast, robotic systems allow for smaller incisions, which not only reduce trauma to the body but also lead to quicker recoveries. Patients can often return to their daily activities much sooner than they would after traditional surgery. This shift towards less invasive techniques is particularly beneficial for patients who are elderly or have underlying health conditions, as it significantly lowers the risks associated with surgery.
However, the journey to fully integrating robotic surgery into the healthcare system is not without its challenges. Training healthcare professionals to effectively use these advanced systems is crucial. Surgeons need to undergo extensive training to become proficient in operating robotic systems, which can be a time-consuming and costly process. Moreover, the implementation of these technologies in healthcare facilities requires significant investment, not just in the robotic systems themselves, but also in the necessary infrastructure and ongoing maintenance. Despite these challenges, the potential of robotic surgery to transform patient care is undeniable.
There are several types of robotic systems utilized in surgeries today, each designed for specific procedures and offering unique features. Some of the most prominent systems include:
- Da Vinci Surgical System: This leading platform enhances surgical capabilities, allowing for highly complex procedures to be performed with precision.
- Versius Surgical System: Known for its versatility, this system adapts to various surgical needs, making it a valuable tool in the operating room.
As robotic systems continue to evolve, we can expect even more innovative solutions that will further enhance surgical practices. The integration of artificial intelligence into these systems is paving the way for smarter surgeries, where robots can assist in decision-making processes during operations, potentially leading to even better patient outcomes.
In conclusion, robotic surgery is not just a glimpse into the future; it's already here, reshaping the way surgeries are performed. As technology advances and more healthcare providers adopt these systems, the benefits for patients will only continue to grow. The prospect of safer, more efficient surgeries is an exciting development that promises to enhance the overall quality of healthcare.
Q: What are the advantages of robotic surgery compared to traditional surgery?
A: Robotic surgery offers several advantages, including reduced recovery times, less pain, minimal scarring, and enhanced precision during procedures.
Q: Are there risks associated with robotic surgery?
A: While robotic surgery is generally considered safe, as with any surgical procedure, there are potential risks. These can include complications related to anesthesia, bleeding, or infection, though they are typically lower than in traditional surgeries.
Q: How long does it take to recover from robotic surgery?
A: Recovery times can vary depending on the type of surgery performed, but patients often experience shorter recovery periods compared to traditional surgery, allowing them to return to their normal activities more quickly.
Types of Robotic Systems
In the rapidly evolving landscape of healthcare, robotic systems are becoming integral tools in surgical procedures. These systems are not one-size-fits-all; rather, they are designed with specific functionalities to cater to various medical needs. Understanding the different types of robotic systems can illuminate how they enhance surgical precision and patient outcomes.
At the forefront of these innovations is the Da Vinci Surgical System, a pioneering platform that has transformed minimally invasive surgery. This system employs advanced robotic arms controlled by a surgeon sitting at a console, allowing for greater dexterity and precision than traditional methods. The Da Vinci system is particularly effective in urology, gynecology, and cardiothoracic surgeries, providing surgeons with enhanced visualization and control over complex procedures.
Another notable system is the Versius Surgical System, which stands out for its versatility. Designed for a range of surgical applications, Versius allows surgeons to perform procedures in a more ergonomic and adaptable manner. Its modular design enables easy setup and repositioning during surgeries, making it a flexible option for operating rooms. Surgeons can engage with the system in a way that feels natural, which can lead to better outcomes and shorter recovery times for patients.
Beyond these, there are several other robotic systems tailored for specific surgical needs. For instance, the MAKO Robotic-Arm Assisted Surgery System specializes in orthopedic procedures, particularly hip and knee replacements. By utilizing 3D imaging and robotic assistance, it allows for precise bone cuts and implant placement, which can significantly enhance the longevity of joint replacements.
Similarly, the ROSATM Surgical System is designed for neurosurgery, providing surgeons with enhanced visualization and precision when operating on delicate structures of the brain and spine. This system integrates advanced imaging technologies to aid in navigating complex anatomical pathways, ensuring patient safety and surgical success.
As we can see, the landscape of robotic systems in surgery is diverse and continually advancing. Each system is engineered to address specific challenges in surgical procedures, ultimately aiming to improve patient care and recovery. As these technologies continue to develop, we can expect even greater innovations that will redefine the surgical experience.
- What is the primary benefit of robotic surgery?
The primary benefit of robotic surgery is its ability to perform minimally invasive procedures with greater precision, leading to reduced recovery times and less postoperative pain for patients.
- Are robotic surgeries safe?
Yes, robotic surgeries are generally safe. They are performed by trained surgeons who utilize advanced technology to enhance their capabilities, ensuring high standards of patient safety.
- How does AI enhance robotic surgery?
AI enhances robotic surgery by providing data analysis and real-time feedback, improving the surgeon's decision-making process and the overall efficiency of the surgical procedure.

Da Vinci Surgical System
The has become a cornerstone in the realm of robotic-assisted surgeries, revolutionizing the way complex procedures are performed. This sophisticated platform provides surgeons with enhanced precision, flexibility, and control that traditional surgical methods simply cannot match. Imagine a surgeon operating with the dexterity of a pianist playing a grand piano, where every movement is amplified and fine-tuned for optimal performance. This is the essence of the Da Vinci system.
One of the most significant advantages of the Da Vinci Surgical System is its ability to perform minimally invasive surgeries. This means smaller incisions, less pain, and quicker recovery times for patients. In fact, studies have shown that patients who undergo surgeries with the Da Vinci system often experience:
- Reduced blood loss
- Shorter hospital stays
- Fewer complications
- Quicker return to normal activities
These benefits are not just statistics; they translate into real-world improvements in patient outcomes. The system utilizes a 3D HD vision system that provides surgeons with a magnified view of the surgical site, allowing for unparalleled visualization of critical structures. This clarity is crucial when navigating delicate areas of the body, such as the prostate, heart, or kidneys.
Moreover, the Da Vinci system is versatile, being applicable in a variety of surgical specialties, including:
- Urology
- Gynecology
- Cardiac surgery
- General surgery
Each of these fields benefits from the precision and control that the Da Vinci system offers, making complex procedures safer and more effective. For instance, in prostatectomies, the robotic system allows for nerve-sparing techniques that can significantly improve postoperative quality of life.
However, it is essential to recognize that the Da Vinci Surgical System is not without its challenges. The cost of the system and its maintenance can be substantial, which may limit its availability in some healthcare facilities. Additionally, surgeons require extensive training to operate the system effectively, ensuring that they can harness its full potential without compromising patient safety.
In conclusion, the Da Vinci Surgical System represents a remarkable advancement in surgical technology, combining robotics with human skill to achieve outcomes that were once thought impossible. As healthcare continues to evolve, systems like Da Vinci will play an increasingly vital role in shaping the future of surgery, enhancing both the capabilities of surgeons and the experiences of patients.
- What is the Da Vinci Surgical System?
The Da Vinci Surgical System is a robotic surgical platform that enhances the capabilities of surgeons, allowing for minimally invasive procedures with greater precision.
- What are the benefits of using the Da Vinci system?
Benefits include reduced blood loss, shorter hospital stays, fewer complications, and quicker recovery times for patients.
- What types of surgeries can be performed with the Da Vinci system?
The system is used in various specialties, including urology, gynecology, cardiac surgery, and general surgery.
- Is training required to use the Da Vinci system?
Yes, surgeons must undergo extensive training to operate the Da Vinci system effectively and safely.

Versius Surgical System
The stands out as a remarkable innovation in the realm of robotic surgery, designed to enhance the versatility and effectiveness of surgical procedures. Unlike traditional robotic systems that may be cumbersome or limited in their application, Versius is engineered with a modular approach, allowing for a more adaptable setup in the operating room. This flexibility means that surgeons can easily configure the system according to the specific needs of each procedure, making it an invaluable tool in various surgical specialties.
One of the key features of the Versius system is its compact design. It is significantly smaller than many other robotic surgical systems, which not only saves space in the operating theater but also allows for easier maneuverability. This aspect is particularly beneficial in smaller hospitals or clinics where space is at a premium. Additionally, the system's design promotes ergonomic positioning for the surgical team, reducing fatigue during long procedures and enhancing overall performance.
Versius is equipped with advanced robotic arms that provide a high degree of precision and control. These arms can replicate the natural movements of a surgeon's hands, allowing for intricate procedures to be performed with unparalleled accuracy. Moreover, the system offers a wide range of instruments that can be easily swapped out during surgery, giving surgeons the tools they need without delay. This adaptability not only improves surgical outcomes but also enhances patient safety by minimizing the time spent under anesthesia.
When comparing Versius to other robotic systems, several advantages emerge:
- Enhanced Versatility: Its modular design allows for use in a variety of surgical specialties, from gynecology to urology.
- Improved Patient Outcomes: Studies have shown that procedures performed with Versius lead to reduced recovery times and lower complication rates.
- Cost-Effectiveness: The system's design can potentially lower operational costs due to its ease of use and maintenance.
In conclusion, the Versius Surgical System is not just another robotic surgical tool; it represents a shift towards more patient-centered care in the operating room. By offering surgeons the ability to customize their approach to each individual procedure, Versius is paving the way for a future where robotic surgery becomes even more integral to modern medicine. As healthcare continues to evolve, systems like Versius will play a crucial role in enhancing surgical precision, improving patient outcomes, and streamlining surgical workflows.
- What types of surgeries can be performed with the Versius Surgical System?
The Versius system can be utilized in various surgical specialties, including gynecology, urology, and general surgery. - How does the Versius system improve patient recovery times?
By enabling minimally invasive procedures, the Versius system reduces trauma to the body, leading to quicker recovery and less postoperative pain. - Is the Versius system easy to use for surgeons?
Yes, the system is designed with user-friendliness in mind, featuring intuitive controls and training programs to help surgeons become proficient quickly.
Training and Implementation
Training healthcare professionals to effectively use robotic systems is crucial for the successful integration of these advanced technologies into clinical practice. Imagine stepping into a high-tech cockpit where every button and lever has a purpose; that's what it feels like for surgeons when they first encounter robotic surgical systems. The learning curve can be steep, but with the right training programs, healthcare providers can master these tools and enhance patient outcomes.
Implementation of robotic systems is not just about the technology; it involves a comprehensive strategy that includes training, workflow integration, and ongoing support. Hospitals must invest in tailored training programs that not only teach the technical skills needed to operate robotic systems but also emphasize the importance of teamwork and communication in the operating room. After all, a surgical team is like an orchestra, where each member plays a vital role in achieving harmony.
One of the primary challenges in training is ensuring that all team members—from surgeons to nurses—are on the same page. This is where simulation-based training comes into play. Using virtual reality and simulation tools, healthcare professionals can practice procedures in a risk-free environment, allowing them to gain confidence before performing actual surgeries. This method is akin to a pilot practicing in a flight simulator before taking to the skies.
Moreover, ongoing education is essential. As technology advances, so too must the skills of healthcare providers. Regular workshops and refresher courses can help maintain high standards of care and ensure that staff are up-to-date with the latest robotic techniques. The goal is to create a culture of continuous learning where healthcare professionals feel empowered to embrace innovation.
To illustrate the training process, here’s a simplified overview of the key phases involved in implementing robotic systems:
| Phase | Description |
|---|---|
| Assessment | Evaluate the needs of the surgical team and identify suitable robotic systems. |
| Training | Conduct hands-on training sessions, including simulation exercises. |
| Implementation | Integrate robotic systems into the surgical workflow, ensuring all team members are comfortable. |
| Evaluation | Monitor outcomes and gather feedback to refine training and procedures. |
In conclusion, the successful training and implementation of robotic systems in healthcare depend on a multifaceted approach that prioritizes education, teamwork, and continuous improvement. By investing in robust training programs and fostering an environment of collaboration, healthcare facilities can harness the full potential of robotic technologies, ultimately leading to better patient care and enhanced surgical precision.
- What is the importance of training for robotic surgery?
Training ensures that healthcare professionals are skilled in using robotic systems, which leads to improved surgical outcomes and patient safety. - How long does it take to train a surgeon to use robotic systems?
The duration of training varies, but it typically ranges from a few weeks to several months, depending on the complexity of the system and the individual’s prior experience. - Are there any risks associated with robotic surgery?
While robotic surgery is generally safe, risks include complications from anesthesia, bleeding, and infection, similar to traditional surgery. - How can hospitals ensure the successful implementation of robotic systems?
By conducting thorough assessments, providing comprehensive training, and fostering a culture of continuous learning, hospitals can ensure successful implementation.

AI in Patient Monitoring
Artificial Intelligence (AI) is making significant strides in the realm of patient monitoring, ushering in a new era of healthcare where real-time data analysis is not just a luxury but a necessity. Imagine a world where healthcare providers are alerted to potential health issues before they escalate, all thanks to the power of AI. This technology analyzes vast amounts of patient data, including vital signs, lab results, and even lifestyle choices, to detect anomalies that may go unnoticed by human eyes.
One of the most exciting aspects of AI in patient monitoring is its ability to enhance patient safety. For instance, AI algorithms can predict adverse events such as heart attacks or strokes by recognizing patterns in the data. This proactive approach allows healthcare professionals to intervene earlier, potentially saving lives. Moreover, AI systems can continuously monitor patients, providing an ongoing assessment of their health status without the need for constant human supervision. This means that healthcare providers can focus on delivering care rather than sifting through mountains of data.
Wearable technology is at the forefront of this revolution. Devices like smartwatches and fitness trackers are no longer just trendy gadgets; they are powerful tools equipped with AI capabilities that enable continuous health monitoring. These wearables can track a variety of metrics, such as heart rate, blood pressure, and even sleep patterns. This data is invaluable for managing chronic conditions like diabetes and hypertension. By providing patients and doctors with real-time insights, these devices empower individuals to take charge of their health.
Furthermore, the integration of AI in telemedicine platforms is transforming how remote patient monitoring is conducted. Patients living in rural or underserved areas can now receive high-quality care without the need to travel long distances. AI facilitates better communication between patients and healthcare providers, ensuring that any concerns are addressed promptly. For example, through AI-driven telehealth applications, patients can share their health data directly with their doctors, who can then provide personalized recommendations based on the latest information.
However, while the benefits of AI in patient monitoring are substantial, it is crucial to address the accompanying challenges. As we embrace these technologies, we must also ensure that they are implemented responsibly and equitably. This includes training healthcare professionals to use AI tools effectively and ensuring that patients are informed about how their data is being used. Only then can we fully harness the potential of AI to improve patient care and outcomes.
| Benefit | Description |
|---|---|
| Real-Time Monitoring | Continuous assessment of patient health, allowing for immediate intervention when necessary. |
| Data-Driven Insights | AI analyzes large datasets to identify trends and predict potential health issues. |
| Improved Communication | Facilitates better interaction between patients and healthcare providers through telemedicine. |
| Empowerment | Patients can actively manage their health with insights gained from wearable devices. |
- What types of data do AI systems analyze in patient monitoring?
AI systems analyze a variety of data, including vital signs, lab results, and patient-reported data from wearables. - How does wearable technology improve patient outcomes?
Wearable technology provides real-time health data, enabling timely interventions and better management of chronic conditions. - Can AI replace healthcare providers in patient monitoring?
No, AI is designed to assist healthcare providers by enhancing their capabilities, not to replace them. - What are the ethical concerns related to AI in patient monitoring?
Concerns include data privacy, consent, and the potential for bias in AI algorithms.

Wearable Technology
Wearable technology is truly revolutionizing the way we monitor our health. Imagine having a personal health assistant that fits right on your wrist or in your pocket! These devices, equipped with advanced AI capabilities, are not just trendy gadgets; they are powerful tools that provide continuous health monitoring, making them invaluable for managing chronic conditions.
One of the standout features of wearable technology is its ability to collect real-time data. For instance, devices like smartwatches and fitness trackers can monitor your heart rate, track your sleep patterns, and even analyze your physical activity levels. This data can be crucial for individuals with conditions such as diabetes or hypertension, as it allows for proactive management of their health. By alerting users to irregularities, these wearables act as an early warning system, potentially preventing serious health issues before they escalate.
Moreover, the integration of AI in these devices enhances their functionality. AI algorithms can analyze the collected data to identify trends and provide personalized insights. For example, if your wearable detects a pattern of elevated heart rates during specific activities, it can suggest modifications to your exercise routine or alert you to consult a healthcare professional. This level of personalized care is not only empowering for patients but also fosters a more engaged approach to health management.
Furthermore, the benefits of wearable technology extend beyond individual users. Healthcare providers can leverage the data collected from wearables to gain a comprehensive view of a patient’s health over time. This continuous stream of information can improve the accuracy of diagnoses and inform treatment plans. By having access to real-time data, doctors can make more informed decisions and provide timely interventions, ultimately leading to better health outcomes.
However, while the advantages are clear, it’s essential to acknowledge the challenges that come with wearable technology. Issues such as data privacy and the need for user engagement are significant. Patients must be educated on how to use these devices effectively and understand the importance of data security. As we embrace this technological advancement, it’s crucial to ensure that patients feel confident in the privacy and security of their health information.
In conclusion, wearable technology represents a significant leap forward in healthcare innovation. By empowering individuals to take charge of their health and providing healthcare professionals with valuable data, these devices are paving the way for a more proactive and personalized approach to healthcare. As we continue to explore the potential of AI in wearable tech, the future looks bright for both patients and providers alike.
- What types of wearable technology are available? Wearable technology includes smartwatches, fitness trackers, smart clothing, and health monitors.
- How does wearable technology improve health monitoring? It provides real-time data on various health metrics, enabling proactive management of health conditions.
- Are there any privacy concerns with wearable devices? Yes, data privacy is a significant concern, and users should be aware of how their data is used and protected.
- Can wearable technology replace traditional medical devices? While wearables can enhance monitoring, they are not a complete replacement for traditional medical devices but rather a complementary tool.

Telemedicine Integration
In today's fast-paced world, telemedicine has emerged as a game-changer in the healthcare landscape, especially when paired with the power of artificial intelligence (AI). Imagine being able to consult with a doctor from the comfort of your home, without the hassle of waiting rooms or long commutes. That's the reality that telemedicine brings to the table. By integrating AI into telemedicine platforms, healthcare providers can offer a more responsive and efficient service, ensuring that patients receive timely care and attention.
One of the standout features of AI in telemedicine is its ability to analyze patient data in real-time. This means that as patients share their symptoms and medical history during a virtual consultation, AI can assist healthcare professionals by providing relevant insights and recommendations. For instance, if a patient reports symptoms that align with a specific condition, AI can quickly pull up the latest research and treatment protocols, allowing the provider to make informed decisions on the spot.
Furthermore, the integration of AI into telemedicine platforms enhances communication between patients and healthcare providers. With features like chatbots and virtual assistants, patients can receive immediate responses to their queries, schedule appointments, or even get reminders for medication. This not only improves patient engagement but also helps in reducing the burden on healthcare systems by streamlining administrative tasks.
However, the implementation of AI in telemedicine isn't without its challenges. For one, there are concerns about the digital divide—not everyone has equal access to technology or the internet, which can hinder the effectiveness of telemedicine in certain populations. Additionally, the reliance on AI raises questions about the quality of care. Can a virtual consultation truly replace the personal touch of an in-person visit? While AI can provide valuable support, it’s essential to maintain a balance between technology and human interaction.
Despite these challenges, the potential benefits of telemedicine integration with AI are immense. It can help in managing chronic conditions, providing mental health support, and even triaging patients before they reach the hospital. The future of healthcare is undoubtedly leaning towards a more connected and technologically advanced model, where patients can receive care anytime, anywhere.
- What is telemedicine? Telemedicine refers to the use of technology to provide healthcare services remotely, allowing patients to consult with healthcare providers via video calls, phone calls, or messaging.
- How does AI enhance telemedicine? AI enhances telemedicine by analyzing patient data in real-time, improving communication, and providing insights that help healthcare providers make informed decisions.
- Are there any challenges with telemedicine integration? Yes, challenges include the digital divide, concerns about the quality of care, and the need for patient data privacy and security.
- Can telemedicine replace in-person visits? While telemedicine offers many benefits, it may not fully replace in-person visits, especially for complex medical conditions that require physical examinations.
Ethical Considerations
As we delve deeper into the integration of artificial intelligence (AI) and robotics in healthcare, it’s crucial to confront the ethical considerations that accompany these advancements. While the potential benefits are enormous, the implications for patient privacy, consent, and the overall decision-making process cannot be overlooked. Imagine a world where a robot performs surgery on you or an AI analyzes your medical history to provide personalized treatment plans. Sounds futuristic, right? But with such innovations come significant responsibilities.
One of the most pressing issues is data privacy. In an era where information is power, ensuring that patient data remains confidential is paramount. Healthcare providers must navigate the intricate balance between utilizing AI for enhanced patient care and protecting sensitive information from breaches. The potential for data leaks or unauthorized access to personal health records poses a significant threat. Therefore, implementing robust security measures is non-negotiable. Providers must adopt comprehensive strategies that include:
- Encryption of patient data
- Regular audits of data access
- Staff training on data handling protocols
Another critical aspect is the potential for bias in AI algorithms. AI systems learn from existing data, which means they can inadvertently inherit biases present in that data. For instance, if an AI model is trained predominantly on data from a specific demographic, it may not perform effectively for patients outside that group. This could lead to disparities in healthcare delivery, where certain populations receive subpar care. Addressing this issue requires a dedicated effort to ensure that AI systems are trained on diverse datasets, reflecting the varied demographics of the patient population.
Moreover, the ethical implications extend to informed consent. Patients must be fully aware of how their data will be used, especially when AI systems are involved in their diagnosis or treatment. Transparency is key; patients should have the right to understand the algorithms that influence their care. This raises the question: How much do patients really know about AI's role in their healthcare? It’s essential for healthcare providers to foster an environment where patients feel comfortable asking questions and voicing concerns about AI technologies.
In conclusion, while the integration of AI and robotics in healthcare holds immense promise, it also presents a myriad of ethical challenges. As we continue to explore these technologies, we must prioritize patient rights, data privacy, and equitable care. By addressing these ethical considerations head-on, we can harness the power of AI and robotics to improve healthcare outcomes while safeguarding the trust and well-being of patients.
Q1: What measures are being taken to protect patient data in AI healthcare applications?
A1: Healthcare providers are implementing encryption, regular audits, and staff training to safeguard patient data against breaches.
Q2: How can biases in AI algorithms affect healthcare delivery?
A2: Biases can lead to disparities in care, where certain demographic groups may receive less effective treatment due to the AI being trained on non-diverse datasets.
Q3: Why is informed consent important in the context of AI in healthcare?
A3: Informed consent ensures that patients understand how their data will be used and the role of AI in their treatment, fostering trust and transparency.

Data Privacy
In today's digital age, has become a critical concern, especially in the realm of healthcare where sensitive patient information is routinely collected and analyzed. As artificial intelligence (AI) and robotics become more integrated into healthcare systems, the need to safeguard patient data is paramount. Imagine a world where your personal health information is as vulnerable as a house with no locks; that’s the reality we face if we don’t prioritize data privacy.
With the implementation of AI solutions in healthcare, vast amounts of data are generated and processed. This includes everything from electronic health records (EHRs) to real-time monitoring data from wearable devices. The challenge lies in ensuring that this data is not only used to improve patient outcomes but also protected against unauthorized access and breaches. Here are some key aspects to consider:
- Patient Consent: Patients must be informed about how their data will be used and must give explicit consent for its collection and analysis.
- Data Encryption: Encrypting sensitive information is crucial to prevent unauthorized access during data transmission and storage.
- Access Controls: Implementing stringent access controls ensures that only authorized personnel can access sensitive patient data.
Moreover, the rise of telemedicine and remote monitoring solutions amplifies the need for robust data privacy measures. For instance, when a patient shares their health data through a telemedicine platform, they expect that their information will remain confidential. Any data breach could not only compromise patient privacy but also erode trust in healthcare providers and technology.
Healthcare organizations must also comply with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, which mandates strict guidelines for protecting patient information. Failure to adhere to these regulations can result in severe penalties and a loss of patient trust. Therefore, it is essential for healthcare providers to regularly audit their data privacy practices and ensure they are up to date with the latest regulations and technologies.
In conclusion, while AI and robotics hold immense potential to revolutionize healthcare, they also bring significant challenges regarding data privacy. It's crucial for healthcare providers to prioritize the protection of patient information, ensuring that innovations do not come at the cost of patient trust and safety. Just as we lock our doors at night to keep our homes safe, we must also take the necessary steps to secure our digital health information in this increasingly connected world.
- What measures can healthcare providers take to ensure data privacy?
Healthcare providers can implement encryption, access controls, and regular audits to safeguard patient information. - How does AI impact patient consent?
AI technologies require clear patient consent regarding the collection and use of their data, emphasizing transparency in data practices. - What are the consequences of data breaches in healthcare?
Data breaches can lead to legal penalties, loss of patient trust, and damage to a healthcare provider's reputation.

Bias in AI Algorithms
As we dive deeper into the integration of artificial intelligence in healthcare, one of the most pressing issues we face is the bias inherent in AI algorithms. These biases can stem from various sources, leading to disparities in healthcare delivery that can significantly impact patient outcomes. Imagine a scenario where a diagnostic tool is trained primarily on data from a specific demographic; it may perform exceptionally well for that group but fail to provide accurate results for others. This is not just a theoretical concern; it's a reality that can affect real lives.
The origins of bias in AI algorithms can often be traced back to the data they are trained on. If the training datasets are not diverse, the resulting AI models may reflect the limitations of that data. For example, if an AI system is trained predominantly on data from one ethnic group, it may not recognize symptoms or conditions that manifest differently in other groups. This can lead to missed diagnoses or inappropriate treatment recommendations, ultimately compromising patient safety and equity in healthcare.
To illustrate this point, consider the following factors that contribute to bias in AI algorithms:
- Data Representation: If certain populations are underrepresented in the training data, the AI may not learn to recognize their unique health needs.
- Labeling Bias: The way data is labeled can introduce bias. If human annotators have their own biases, these can be passed on to the AI.
- Algorithmic Design: The design choices made by developers can inadvertently favor certain groups over others, leading to biased outcomes.
Addressing bias in AI is not just about improving technology; it’s about ensuring equitable healthcare for all. Developers and healthcare professionals must work collaboratively to create AI systems that are not only accurate but also fair. This involves rigorous testing of AI algorithms across diverse populations and continuous monitoring of their performance in real-world applications. By prioritizing diversity and inclusivity in both data collection and AI development, we can mitigate these biases and enhance the quality of care for everyone.
Furthermore, regulatory bodies and healthcare organizations need to establish guidelines that promote transparency in AI algorithms. This means being open about how algorithms are developed and the data used, allowing for scrutiny and accountability. After all, in a field as critical as healthcare, we cannot afford to overlook the ramifications of biased algorithms.
In conclusion, while AI has the potential to revolutionize healthcare, we must remain vigilant about the biases that can compromise its effectiveness. By addressing these biases head-on, we can harness the power of AI to create a more equitable healthcare system that serves all patients, regardless of their background.
Frequently Asked Questions
- What role does AI play in diagnostics?
AI is transforming diagnostics by rapidly analyzing vast amounts of medical data, identifying patterns, and delivering results much faster than traditional methods. This means quicker disease detection and more accurate patient diagnoses, which can significantly enhance patient outcomes.
- How does robotic surgery improve patient care?
Robotic surgery enhances patient care through its precision and minimally invasive techniques. These surgeries often lead to reduced recovery times, less pain, and fewer complications, allowing patients to return to their normal lives sooner.
- What are the different types of robotic systems used in surgeries?
There are several types of robotic systems designed for specific surgical procedures, including the Da Vinci Surgical System, known for its advanced capabilities in complex surgeries, and the Versius Surgical System, which offers versatility across various operations. Each system has unique features tailored to improve surgical outcomes.
- How is training conducted for healthcare professionals using robotic systems?
Training for healthcare professionals involves hands-on experience with the robotic systems, simulation-based learning, and mentorship from experienced surgeons. However, challenges can arise, such as the steep learning curve and the need for ongoing education as technology evolves.
- What benefits do wearable technologies provide in healthcare?
Wearable technologies equipped with AI capabilities allow for continuous monitoring of health metrics, enabling patients and healthcare providers to manage chronic conditions more effectively. They provide real-time data that can alert providers to potential health issues before they escalate.
- How does AI enhance telemedicine?
AI enhances telemedicine by improving remote patient monitoring and facilitating better communication between patients and healthcare providers. This is especially beneficial for patients in remote areas, allowing them to receive timely care without needing to travel long distances.
- What are the ethical concerns surrounding AI in healthcare?
As AI and robotics become more integrated into healthcare, ethical concerns such as patient privacy, informed consent, and the potential for biased decision-making arise. It’s crucial to address these issues to ensure equitable and ethical use of technology in patient care.
- How is patient data privacy maintained with AI solutions?
Maintaining patient data privacy involves implementing robust security measures, such as encryption and access controls, to protect sensitive information. It's essential for healthcare providers to prioritize data security to build trust with patients in the digital age.
- What is the issue of bias in AI algorithms?
Bias in AI algorithms can lead to disparities in healthcare delivery, as these algorithms might inherit biases from their training data. It’s vital to develop and implement AI solutions that are equitable and consider diverse patient populations to ensure fair treatment for all.