Decoding the Ethics of AI in Healthcare
As we stand on the brink of a technological revolution, the integration of artificial intelligence (AI) into healthcare is not just a trend; it's a transformative wave reshaping how we approach medical practices. From predictive analytics that can forecast patient outcomes to AI-driven diagnostic tools that enhance accuracy, the potential benefits are staggering. However, with great power comes great responsibility, and this is where the ethical considerations come into play. In this article, we will explore the multifaceted ethical landscape surrounding AI in healthcare, examining its implications, benefits, challenges, and the necessity for responsible implementation.
To appreciate the ethical dilemmas posed by AI in healthcare, we first need to understand what AI actually entails in this context. AI technologies, such as machine learning, natural language processing, and robotic process automation, are being utilized in various applications, including:
- Diagnostics: AI algorithms analyze medical images, lab results, and patient data to assist healthcare professionals in diagnosing diseases more accurately.
- Treatment Planning: AI systems can suggest personalized treatment plans based on a patient's unique genetic makeup and medical history.
- Patient Management: AI tools help in monitoring patient progress and managing chronic conditions through real-time data analysis.
These applications are revolutionizing traditional medical practices by enhancing efficiency, reducing human error, and ultimately improving patient outcomes. However, as we embrace these advancements, we must tread carefully, ensuring that ethical principles guide our journey.
The development and deployment of AI in healthcare are governed by core ethical principles that are crucial in maintaining public trust and ensuring equitable care. These principles include:
- Autonomy: Respecting patient autonomy means acknowledging their right to make informed decisions about their own healthcare.
- Beneficence: This principle emphasizes the importance of acting in the best interest of the patient.
- Non-maleficence: Often summarized as "do no harm," this principle underlines the necessity of preventing harm to patients.
- Justice: This principle focuses on fairness in healthcare delivery, ensuring that all patients have equal access to AI technologies.
Understanding and implementing these ethical principles is vital for the responsible use of AI in healthcare, as they serve as the foundation for trust between patients and healthcare providers.
One of the most significant ethical considerations in AI-driven healthcare is the concept of patient autonomy. Patients have the right to make informed choices about their treatment options, and AI tools can both enhance and complicate this process. With the rise of AI, the question arises: how do we ensure that patients truly understand the role of AI in their healthcare? This leads us to the intricate web of informed consent.
Obtaining informed consent in the context of AI applications presents unique challenges. The complexity of AI algorithms can lead to a lack of transparency, leaving patients confused about how their data is being used and how decisions are being made. For instance, if a patient is told that an AI system will determine their treatment plan, they might not fully grasp the implications of this technology. This lack of understanding can hinder their ability to give truly informed consent.
On the flip side, AI can significantly empower patient choice by providing personalized treatment options tailored to individual needs. Imagine a scenario where an AI system analyzes a patient's genetic information and medical history to suggest the most effective treatment. This not only enhances the patient's ability to make informed decisions but also respects their fundamental right to autonomy. Still, the challenge remains: how do we balance AI's capabilities with the need for clear communication and understanding?
As we delve deeper into the ethical landscape, we must confront the issue of equity in access to AI technologies. The potential for disparities in healthcare delivery is a pressing concern. Not everyone has equal access to advanced AI tools, which can exacerbate existing inequalities. The ethical obligation to ensure fair access for all patients is paramount, as we strive for a healthcare system that serves everyone, regardless of their background or socioeconomic status.
Another critical ethical consideration in AI healthcare applications is data privacy. With the vast amounts of sensitive patient information being processed by AI systems, safeguarding this data is essential. The risks associated with data breaches can lead to significant harm, both to patients and healthcare providers. Thus, ensuring robust data security measures is not just a technical requirement; it's an ethical imperative.
To navigate these ethical challenges, existing regulations governing AI in healthcare must be examined. Are they effective in protecting patient rights and ensuring ethical standards? The answer isn't straightforward, but it is clear that continuous evaluation and adaptation of these frameworks are necessary to keep pace with technological advancements.
As we look to the future, the ethical landscape of AI in healthcare will undoubtedly evolve. New challenges will emerge as technology advances, and it is crucial to remain vigilant. The integration of AI into medical practice deepens, and we must continually reflect on the ethical implications of our choices.
Q: What are the main ethical concerns regarding AI in healthcare?
A: The primary ethical concerns include patient autonomy, informed consent, data privacy, and equitable access to AI technologies.
Q: How does AI impact patient decision-making?
A: AI can enhance patient decision-making by providing personalized treatment options, but it can also complicate the process if patients do not fully understand how AI systems work.
Q: Are there regulations in place for AI in healthcare?
A: Yes, there are regulations governing AI in healthcare, but their effectiveness in protecting patient rights and ensuring ethical standards requires ongoing assessment.

Understanding AI in Healthcare
Artificial Intelligence (AI) is transforming the healthcare landscape in ways that were once thought to be the stuff of science fiction. Imagine a world where machines can analyze thousands of medical images in the blink of an eye, or where algorithms can predict patient outcomes with astonishing accuracy. This isn’t just a dream; it’s happening right now. AI technologies are being integrated into various aspects of healthcare, from diagnostics to treatment plans, and even patient management. The potential to revolutionize traditional medical practices is immense, and understanding these technologies is crucial for both healthcare professionals and patients alike.
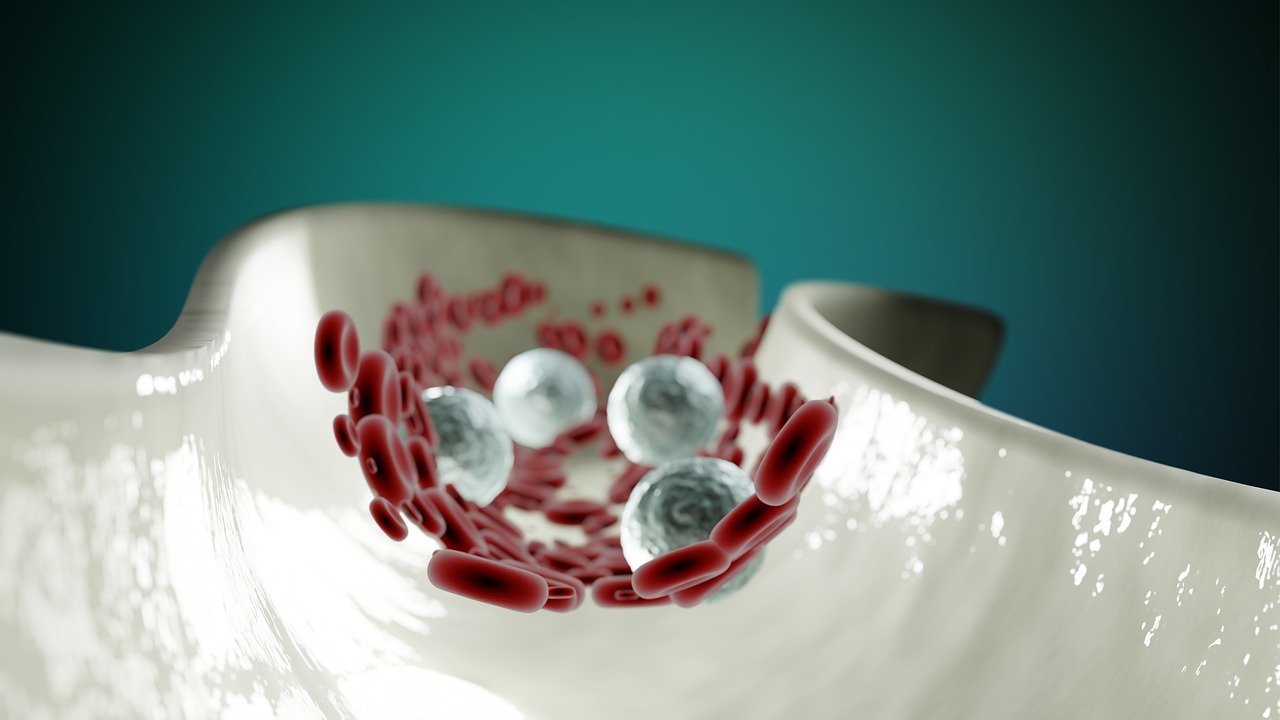
At its core, AI in healthcare encompasses a range of technologies, including machine learning, natural language processing, and robotics. These tools are designed to assist healthcare providers in making more informed decisions, improving patient care, and enhancing operational efficiency. For instance, machine learning algorithms can sift through vast amounts of data to identify patterns that humans might miss. This capability is particularly useful in diagnostics, where AI can help detect diseases such as cancer at an early stage, leading to better outcomes for patients.
Moreover, AI is not just limited to diagnostics. It plays a significant role in treatment personalization. By analyzing patient data, AI can help create tailored treatment plans that consider individual patient needs, preferences, and responses to previous therapies. This personalized approach can enhance the effectiveness of treatments, reduce side effects, and ultimately lead to improved patient satisfaction. In fact, studies have shown that AI-driven personalized treatment plans can lead to a significant increase in treatment adherence among patients.
Furthermore, AI is transforming patient management by streamlining administrative tasks and improving communication between patients and healthcare providers. For example, AI-powered chatbots can answer patient queries, schedule appointments, and provide medication reminders, allowing healthcare professionals to focus on what they do best—caring for patients. This not only improves the patient experience but also increases the efficiency of healthcare systems.
However, while the benefits of AI in healthcare are substantial, it is essential to approach its implementation with caution. The integration of AI technologies raises questions about data privacy, security, and the potential for bias in algorithms. These challenges must be addressed to ensure that the deployment of AI in healthcare is ethical and equitable. As we continue to explore the capabilities of AI, it is crucial for stakeholders to engage in discussions about its implications and to establish guidelines that prioritize patient welfare and ethical standards.
In summary, the understanding of AI in healthcare is a multifaceted topic that encompasses a variety of technologies and applications. As we embrace this technological revolution, it is vital to remain vigilant about the ethical considerations that accompany it. By doing so, we can harness the power of AI to enhance patient care while safeguarding the principles that underpin medical ethics.
- What is AI in healthcare? AI in healthcare refers to the use of artificial intelligence technologies to improve diagnostics, treatment plans, and patient management.
- How does AI enhance diagnostics? AI can analyze large datasets and identify patterns, allowing for earlier and more accurate disease detection.
- What are the ethical concerns surrounding AI in healthcare? Key concerns include data privacy, algorithmic bias, and the need for informed consent from patients.
- Can AI replace healthcare professionals? While AI can assist healthcare professionals, it is not intended to replace them; rather, it aims to enhance their capabilities.

Ethical Principles in AI
When diving into the world of artificial intelligence (AI) in healthcare, it’s crucial to anchor ourselves in the ethical principles that guide its development and application. These principles are not just abstract concepts; they form the backbone of what it means to deliver care in a responsible and humane manner. Among the most significant are autonomy, beneficence, non-maleficence, and justice. Each of these principles plays a pivotal role in shaping how AI technologies are integrated into healthcare systems, ensuring that they enhance patient care rather than undermine it.
Autonomy is about empowering patients to make informed decisions regarding their health. In a landscape increasingly dominated by AI, it's essential to ensure that patients retain control over their healthcare choices. Imagine a scenario where AI tools suggest treatment options based on vast datasets; while this can be incredibly beneficial, it raises questions about how much influence these tools should have on patient decisions. Are patients truly informed, or are they simply following AI recommendations without understanding the underlying processes?
Next, we have beneficence, which emphasizes the moral obligation to act in the best interests of patients. AI has the potential to revolutionize healthcare by providing tailored treatment plans, predicting outcomes, and identifying potential health risks before they escalate. However, the challenge lies in ensuring that these technologies are designed and implemented with the patient’s best interest at heart. It’s not enough for AI to be effective; it must also be ethically sound.
Non-maleficence is another cornerstone principle, which dictates that healthcare providers must avoid causing harm. With AI, this can be tricky. For example, if an AI algorithm misdiagnoses a condition due to biased training data, it could lead to harmful outcomes for patients. Therefore, developers must rigorously test and validate their algorithms to mitigate any potential harm. This principle serves as a reminder that while technology can enhance care, it must be approached with caution and responsibility.
Finally, we have the principle of justice, which calls for fairness in healthcare access and treatment. As AI technologies become more prevalent, there is a risk that disparities in access could widen. For instance, if only affluent healthcare systems can afford advanced AI tools, this could lead to unequal treatment outcomes. It’s vital to advocate for policies that ensure equitable access to AI innovations, so every patient, regardless of their socioeconomic status, can benefit from these advancements.
In summary, the ethical principles of autonomy, beneficence, non-maleficence, and justice are not just theoretical frameworks; they are essential guidelines that must steer the development and application of AI in healthcare. As we continue to explore the potential of AI technologies, we must remain vigilant and committed to these principles to ensure that the benefits of AI are realized without compromising ethical standards.
- What is the role of ethics in AI healthcare? Ethics in AI healthcare ensures that technologies are designed and used in ways that respect patient rights and promote fair treatment.
- How does autonomy affect patient care with AI? Autonomy allows patients to make informed decisions about their treatment, ensuring they understand the role of AI in their care.
- What are the risks of AI in healthcare? Risks include misdiagnosis, data privacy issues, and potential biases in AI algorithms that could lead to unequal treatment.
- How can we ensure justice in AI healthcare? Ensuring justice involves creating policies that promote equitable access to AI technologies for all patients.

Autonomy and Patient Consent
In the realm of healthcare, patient autonomy stands as a fundamental principle, akin to the North Star guiding ethical medical practices. When we talk about autonomy, we’re essentially referring to a patient’s right to make informed decisions about their own health care. With the advent of artificial intelligence (AI) in healthcare, this concept takes on new dimensions, bringing both opportunities and challenges. How does AI fit into the picture of patient autonomy? Can it enhance or hinder a patient's ability to make choices about their own treatment? These are questions that deserve our attention.
AI tools can provide patients with a wealth of information, from diagnostic results to treatment options. Imagine having a virtual assistant that not only explains your condition but also offers tailored treatment plans based on your unique genetic makeup and lifestyle. Sounds great, right? However, there’s a flip side to this shiny coin. The more complex the AI systems become, the harder it can be for patients to fully understand how these systems work and how decisions are made. This is where informed consent comes into play.
Informed consent isn’t just a checkbox to tick off; it’s a dynamic process that ensures patients understand the implications of their choices. When AI is involved, the challenge intensifies. Patients must grasp not only the potential benefits of AI-driven solutions but also the risks and limitations. For instance, if a patient is presented with a treatment option recommended by an AI system, they need to be aware of how the AI arrived at that recommendation. Was it based on a vast database of similar cases? Or was it influenced by biased data? Transparency in AI algorithms is crucial for maintaining patient trust and autonomy.
But let’s dive deeper. What does it mean for patients to truly empower their choices in an AI-driven environment? The answer lies in striking a balance. AI should serve as a tool that enhances patient decision-making rather than replacing it. By providing personalized insights, AI can help patients weigh their options more effectively. For example, an AI system could analyze a patient’s medical history and suggest potential treatments, but ultimately, the decision should rest with the patient. This empowerment fosters a sense of agency and responsibility over one’s health, reinforcing the core tenets of autonomy.
To facilitate this empowerment, healthcare providers must prioritize clear communication. Patients should feel comfortable asking questions and expressing concerns about AI recommendations. This dialogue can help demystify AI and encourage patients to engage actively in their healthcare decisions. After all, a well-informed patient is a powerful patient.
In summary, while AI holds the potential to revolutionize healthcare, it is imperative to ensure that patient autonomy remains at the forefront. By understanding the complexities of informed consent and fostering open communication, we can harness the power of AI without compromising the fundamental rights of patients. The road ahead may be fraught with challenges, but with a commitment to ethical practices, we can navigate this new landscape together.

Informed Consent Challenges
When we think about informed consent in healthcare, it’s like opening a door to a room filled with intricate puzzles. Each puzzle piece represents a unique challenge, particularly when it comes to integrating artificial intelligence (AI) into medical practices. One of the primary hurdles is the complexity of algorithms used in AI systems. Patients often find it difficult to understand how these algorithms work, which can lead to confusion and mistrust. Imagine trying to explain a complicated recipe to someone who has never cooked before; the more complex the recipe, the harder it is for them to grasp the essential steps. Similarly, AI systems can be daunting for patients who are not tech-savvy.
Moreover, there is a significant challenge regarding the transparency of AI systems. Many algorithms operate as "black boxes," meaning that even the developers may not fully understand how certain decisions are made. This lack of transparency raises ethical questions about whether patients can genuinely give informed consent when they don’t have a clear picture of how their data is being used or how decisions regarding their care are being made. For instance, if an AI tool recommends a specific treatment, how can patients trust that recommendation if they don't understand the underlying reasoning?
Additionally, the potential for misunderstandings about AI's role in patient care can complicate the informed consent process. Patients may overestimate the capabilities of AI, believing it to be infallible, or underestimate it, thinking that it could replace human judgment entirely. This can lead to unrealistic expectations or fear of being sidelined in their healthcare journey. It’s crucial for healthcare providers to bridge this knowledge gap by simplifying complex information and ensuring that patients feel comfortable asking questions.
To address these challenges, a multi-faceted approach is necessary. Healthcare providers can consider the following strategies:
- Education and Training: Offering workshops or informational sessions can help demystify AI technologies for patients.
- Clear Communication: Using plain language to explain how AI tools work and their implications in treatment can foster understanding.
- Patient Involvement: Encouraging patients to participate in discussions about their care can empower them to make informed decisions.
In conclusion, while the integration of AI in healthcare holds great promise, it also presents significant challenges in obtaining informed consent. By addressing these challenges head-on, healthcare providers can ensure that patients remain at the center of their care, fully informed and empowered to make decisions about their health.

Empowering Patient Choice
In the rapidly evolving landscape of healthcare, one of the most exciting prospects offered by artificial intelligence (AI) is its potential to empower patient choice. Imagine a world where every patient has access to personalized treatment options tailored specifically to their unique health profiles. This is not just a pipe dream; it's becoming a reality thanks to AI. By analyzing vast amounts of data, AI can provide insights that help patients make informed decisions about their healthcare.
AI technologies can analyze a patient’s medical history, genetic information, and even lifestyle choices to recommend treatments that are not only effective but also align with the patient’s values and preferences. This level of personalization is akin to having a healthcare assistant who knows you inside out, guiding you through the maze of medical options available. It’s about putting the patient in the driver’s seat, allowing them to steer their own healthcare journey.
However, it’s essential to recognize that empowering patient choice doesn’t mean overwhelming them with information. Instead, AI can distill complex medical data into understandable formats, presenting options clearly and concisely. For instance, consider the following benefits of AI in enhancing patient choice:
- Personalized Recommendations: AI can suggest treatments based on individual patient data, leading to more effective healthcare outcomes.
- Informed Decision-Making: With AI, patients can access information about potential side effects, success rates, and alternative treatments, enabling them to make informed choices.
- Improved Communication: AI tools can facilitate better communication between patients and healthcare providers, ensuring that patients feel heard and understood.
Furthermore, the integration of AI in healthcare can also help address disparities in treatment options. For instance, AI can analyze data from diverse populations to ensure that recommendations are equitable and inclusive. This means that no matter where you come from or what background you have, AI can help ensure that you have access to the best possible treatment options available.
However, while AI has the potential to enhance patient choice, it's crucial to remember that the fundamental right to autonomy must always be respected. Patients should never feel pressured to choose a specific treatment based on AI recommendations alone. Instead, AI should serve as a tool that complements the expertise of healthcare providers, fostering a collaborative environment where patients feel empowered to voice their preferences and concerns.
In conclusion, the role of AI in empowering patient choice is transformative. By providing personalized treatment options and facilitating informed decision-making, AI not only enhances the patient experience but also respects and upholds the values of autonomy and respect. As we continue to navigate this exciting frontier, it is vital that we remain committed to ensuring that the voice of the patient is always at the forefront of healthcare innovations.
- How does AI personalize treatment options for patients? AI analyzes individual patient data, including medical history and genetics, to recommend tailored treatment plans.
- Can AI replace doctors in decision-making? No, AI is designed to assist healthcare providers by providing insights, but the final decision should always involve the patient and their doctor.
- What are the risks associated with AI in healthcare? Risks include data privacy concerns, algorithm biases, and potential misunderstandings regarding AI's recommendations.
- How can patients ensure their data is secure when using AI tools? Patients should inquire about data protection measures and choose healthcare providers that comply with regulations regarding data privacy.

Equity and Access to AI
As we stand on the precipice of a technological revolution in healthcare, the issue of technologies becomes increasingly pressing. Imagine a world where cutting-edge diagnostic tools and personalized treatment plans are available to everyone, regardless of their socioeconomic status. Sounds ideal, right? However, the reality is often starkly different. The integration of AI into healthcare has the potential to widen the gap between those who can afford advanced medical technologies and those who cannot. This disparity raises profound ethical questions about our responsibility to ensure that all patients have fair access to these innovations.
One of the primary concerns is that AI tools are often developed and deployed in ways that favor affluent populations. For instance, hospitals in urban areas with greater resources can invest in sophisticated AI systems that enhance patient care, while rural or underfunded facilities may struggle to keep pace. This creates a scenario where patients in wealthier regions receive superior healthcare services, while those in less affluent areas are left behind. The implications of this inequity are staggering, as it could lead to a two-tiered healthcare system where only the privileged have access to the best that technology has to offer.
Moreover, the algorithms that power AI systems are often trained on datasets that may not represent the diverse populations they serve. This lack of representation can lead to biased outcomes, where certain demographics receive inferior treatment options or are misdiagnosed altogether. For example, if an AI system is primarily trained on data from one ethnic group, it may not perform as effectively for patients from other backgrounds. This not only raises ethical concerns but also poses a significant risk to patient safety.
To address these challenges, we must prioritize equity in AI access by implementing several key strategies:
- Inclusive Data Practices: Ensuring that AI algorithms are trained on diverse datasets that reflect the populations they will serve is critical.
- Community Engagement: Involving underserved communities in the development and implementation of AI technologies can help identify their unique needs and barriers to access.
- Policy Advocacy: Advocating for policies that promote equitable access to AI technologies in healthcare settings is essential for systemic change.
Ultimately, the goal is to create a healthcare system where everyone, regardless of their background or economic status, has access to the benefits of AI. This requires a concerted effort from healthcare providers, policymakers, and technology developers to ensure that equity is at the forefront of AI integration in healthcare. By addressing these disparities head-on, we can harness the power of AI to not only improve patient outcomes but also to foster a more just and equitable healthcare system for all.
Q1: What are the main barriers to accessing AI technologies in healthcare?
A1: The main barriers include socioeconomic disparities, lack of representation in training data, and insufficient infrastructure in rural or underfunded healthcare facilities.
Q2: How can we ensure that AI tools are fair and equitable?
A2: By implementing inclusive data practices, engaging with diverse communities, and advocating for equitable healthcare policies, we can work towards fair AI access.
Q3: Why is patient representation important in AI development?
A3: Patient representation ensures that AI systems are trained on diverse datasets, reducing the risk of biased outcomes and improving the effectiveness of treatment across different populations.

Data Privacy and Security
In the age of artificial intelligence, the healthcare sector is experiencing a seismic shift, but with great power comes great responsibility. As AI technologies become increasingly integrated into healthcare systems, the ethical implications surrounding data privacy and security cannot be overlooked. Imagine a world where your medical history is not just stored but analyzed by intelligent algorithms to predict your health outcomes. Sounds amazing, right? But what happens to your sensitive data during this process? Ensuring the confidentiality and integrity of patient information is paramount, as any breach could have devastating consequences.
At the heart of this discussion is the need for robust data protection measures. Healthcare organizations must adopt comprehensive strategies to secure patient information against unauthorized access and cyber threats. This includes not only implementing state-of-the-art encryption technologies but also fostering a culture of data privacy awareness among healthcare professionals. After all, a chain is only as strong as its weakest link, and human error can often be the Achilles' heel in data security.
Moreover, the ethical obligation to protect patient data extends beyond just safeguarding it; it also involves being transparent about how this data is used. Patients have the right to know who has access to their information and for what purposes. This transparency is crucial in building trust between patients and healthcare providers. A recent study indicated that up to 70% of patients express concerns about how their data is handled, highlighting the need for clear communication regarding data practices.
To address these issues, healthcare organizations can benefit from establishing a comprehensive privacy framework. This framework should include:
- Regular audits of data handling practices
- Employee training programs on data security
- Clear policies on data sharing and usage
- Patient education initiatives on their rights regarding data privacy
In addition to internal measures, collaboration with regulatory bodies is essential. Existing regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, set standards for protecting sensitive patient data. However, as AI technologies evolve, these regulations must also adapt to address new challenges. The balance between innovation and regulation is delicate, and ongoing dialogue among stakeholders is necessary to ensure that ethical standards keep pace with technological advancements.
As we look to the future, the ethical landscape of data privacy and security in AI healthcare applications will continue to evolve. With the rise of new technologies such as blockchain and advanced encryption methods, there is potential for enhanced data security. However, the challenge remains: how do we harness these technologies while ensuring that patient rights are prioritized? It’s a question that will require thoughtful consideration and proactive measures from all parties involved.
- What are the main concerns regarding data privacy in AI healthcare?
Patients worry about unauthorized access to their sensitive medical information and how it may be used without their consent. - How can healthcare organizations improve data security?
By implementing robust encryption, conducting regular audits, and fostering a culture of awareness among staff regarding data privacy. - What role do regulations play in data privacy?
Regulations like HIPAA set standards for protecting patient data, ensuring that healthcare organizations comply with ethical practices.

Regulatory Frameworks
As the integration of artificial intelligence (AI) in healthcare continues to expand, the need for robust regulatory frameworks becomes increasingly critical. These frameworks serve as the backbone for ensuring that AI technologies are developed and deployed responsibly, safeguarding patient rights while promoting innovation. The challenge lies in striking a balance between fostering technological advancement and ensuring ethical standards are met. Without proper regulations, the potential for misuse and ethical dilemmas escalates, which can undermine public trust in AI applications.
Currently, various organizations and governmental bodies are working to establish guidelines and regulations that address the unique challenges posed by AI in healthcare. For instance, the U.S. Food and Drug Administration (FDA) has begun to outline a framework for the evaluation of AI-based medical devices, focusing on safety, effectiveness, and transparency. Similarly, the European Union is in the process of developing comprehensive regulations aimed at ensuring that AI technologies adhere to ethical principles, including respect for human rights and privacy.
One crucial aspect of these regulatory frameworks is the emphasis on accountability. As AI systems are often complex and opaque, establishing clear lines of responsibility becomes vital. This is where the concept of a “human in the loop” comes into play, ensuring that healthcare professionals remain involved in critical decision-making processes. By doing so, we can mitigate the risks associated with algorithmic biases and errors, ultimately enhancing patient safety.
Moreover, regulations must address data privacy and security concerns, particularly given the sensitive nature of healthcare data. Regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. set stringent standards for protecting patient information, but as AI technologies evolve, these laws must adapt accordingly. The introduction of AI into healthcare necessitates a reevaluation of existing privacy laws to ensure they effectively protect patients while allowing for the beneficial use of data in AI systems.
In addition to national regulations, international cooperation is essential for the effective governance of AI in healthcare. As healthcare increasingly transcends borders, harmonizing regulations across different jurisdictions can facilitate the responsible use of AI technologies globally. This can be achieved through collaborative efforts among international organizations, healthcare providers, and technology developers, ensuring that best practices are shared and implemented.
To summarize, the establishment of comprehensive regulatory frameworks is paramount for the ethical integration of AI in healthcare. These frameworks should encompass accountability, data privacy, and international cooperation, paving the way for a future where AI can enhance healthcare delivery while maintaining the highest ethical standards.
- What are the main goals of regulatory frameworks for AI in healthcare?
The primary goals include ensuring patient safety, protecting data privacy, and fostering innovation while maintaining ethical standards. - How do regulatory frameworks impact the development of AI technologies?
They provide guidelines that help developers create safe and effective AI solutions while addressing ethical concerns. - Why is international cooperation important in AI regulation?
Healthcare often crosses borders, and harmonizing regulations can ensure consistent standards and practices globally.
Future Ethical Considerations
As we stand on the brink of a technological revolution in healthcare, the ethical landscape is evolving just as rapidly as the innovations themselves. The integration of artificial intelligence (AI) into medical practice brings with it a host of ethical dilemmas that healthcare professionals, developers, and policymakers must navigate. One of the most pressing concerns is the potential for bias in AI algorithms. If these systems are trained on data that reflects existing inequalities, they could perpetuate and even exacerbate disparities in healthcare access and outcomes. This raises the question: how can we ensure that AI serves to bridge gaps rather than widen them?
Moreover, as AI becomes more autonomous in decision-making processes, we must grapple with the implications for human oversight. Will healthcare providers become overly reliant on AI recommendations, potentially undermining their own clinical judgment? This concern is particularly acute in high-stakes scenarios, such as surgical procedures or critical care situations. It’s crucial that we establish a balance between leveraging AI’s capabilities and maintaining the essential human element in patient care.
Another significant ethical consideration is the transparency of AI systems. Patients have a right to understand how decisions about their health are made, yet many AI algorithms operate as "black boxes," making it challenging to discern how conclusions are reached. This opacity can lead to mistrust among patients, especially if they feel their care is being dictated by an inscrutable machine. As we advance, developing standards for transparency and explainability in AI will be vital to fostering trust and ensuring informed consent.
Additionally, the rapid pace of AI development poses a challenge for regulatory bodies. Current regulations may not adequately address the unique ethical concerns posed by AI in healthcare. As new technologies emerge, there is a pressing need for adaptive regulatory frameworks that can keep pace with innovation. These frameworks must not only protect patient rights but also encourage the responsible development of AI technologies. This leads us to consider: how can we create a regulatory environment that is both flexible and robust enough to handle future advancements?
Finally, the ethical implications of data privacy and security cannot be overlooked. With AI systems relying heavily on vast amounts of patient data, the risk of data breaches and unauthorized access becomes a critical concern. Patients must feel confident that their sensitive information is safeguarded against misuse. Establishing stringent data protection measures and fostering a culture of accountability within healthcare organizations will be essential in addressing these fears.
In conclusion, the future of AI in healthcare is filled with both promise and peril. By actively engaging with these ethical considerations, we can work towards a future where AI enhances healthcare delivery while respecting patient rights and promoting equity. The path forward will require collaboration among technologists, healthcare professionals, ethicists, and patients to create an environment where technology serves humanity, not the other way around.
- What are the main ethical concerns regarding AI in healthcare? The main concerns include bias in algorithms, transparency of decision-making processes, data privacy, and the potential for over-reliance on AI by healthcare providers.
- How can we ensure that AI serves all patients equally? By addressing bias in AI training data and implementing equitable access policies, we can work towards ensuring that AI benefits all patients.
- What role does patient consent play in AI healthcare applications? Informed consent is crucial, as patients need to understand how AI tools will be used in their care and the implications of these technologies on their treatment decisions.
- Are current regulations sufficient to govern AI in healthcare? Many believe that existing regulations may not adequately address the unique challenges posed by AI, highlighting the need for adaptive regulatory frameworks.
- What steps can be taken to protect patient data in AI systems? Implementing robust data protection measures and fostering accountability within healthcare organizations are essential steps to safeguard patient information.
Frequently Asked Questions
- What are the main benefits of using AI in healthcare?
AI in healthcare brings a plethora of benefits! It can enhance diagnostics, streamline treatment plans, and improve patient management. Imagine having a super-smart assistant that helps doctors make more accurate decisions while also personalizing care for patients. This technology can analyze vast amounts of data quickly, leading to better outcomes and a more efficient healthcare system overall.
- How does AI impact patient autonomy and consent?
Great question! Patient autonomy is crucial in healthcare, and AI plays a unique role here. While AI tools can empower patients by providing personalized options, they also raise challenges regarding informed consent. Patients need to understand how AI affects their treatment decisions. It's like having a GPS for your health journey—helpful, but you still want to know where you're going and why!
- What ethical principles guide the use of AI in healthcare?
The ethical landscape of AI in healthcare is guided by principles like autonomy, beneficence, non-maleficence, and justice. These principles ensure that AI technologies are developed and implemented responsibly. Think of them as the moral compass for navigating the complex waters of healthcare technology. They remind us to prioritize patient well-being and fairness in access to care.
- Are there concerns about data privacy with AI in healthcare?
Absolutely! Data privacy is a major concern when it comes to AI in healthcare. With sensitive patient information being processed, the risk of data breaches is a pressing issue. It's like handing your personal diary to someone else—trust is key, and patients must feel secure that their information is protected. Therefore, robust measures need to be in place to safeguard this data.
- What is the role of regulatory frameworks in AI healthcare?
Regulatory frameworks are essential for ensuring that AI technologies in healthcare adhere to ethical standards. They act like traffic lights on a busy road, guiding developers and healthcare providers to operate safely and responsibly. These regulations help protect patient rights and ensure that AI tools are used in a way that benefits everyone, not just a select few.
- What future ethical challenges might arise as AI continues to evolve in healthcare?
As AI technology evolves, so do the ethical challenges. Issues like algorithmic bias, transparency in AI decision-making, and ongoing patient consent will become increasingly important. It's like watching a thrilling movie—you never know what twists and turns are coming! Staying ahead of these challenges will be crucial to ensuring that AI remains a force for good in healthcare.