Advance Healthcare through AI: The Future is Here
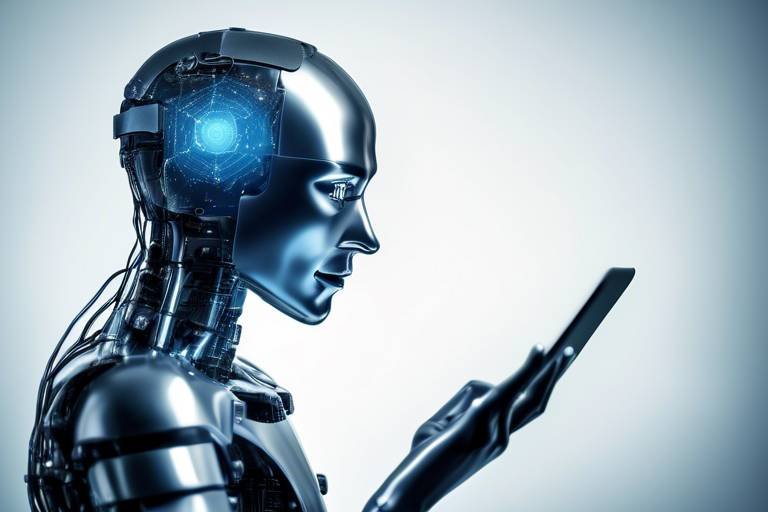
The world of healthcare is on the brink of a revolution, and at the heart of this transformation is artificial intelligence (AI). Imagine a world where diseases are diagnosed with pinpoint accuracy, treatment plans are tailored to individual patients, and drug discovery is expedited—all thanks to the power of AI. This technology isn't just a trend; it's a game changer that promises to redefine how we approach health and wellness. As we dive deeper into this topic, we will explore the myriad ways AI is reshaping healthcare, the challenges it faces, and the incredible potential it holds for the future.
AI has already begun to infiltrate various aspects of healthcare, from diagnostics to treatment and even in administrative tasks. Its ability to process vast amounts of data at lightning speed allows for enhanced decision-making, better patient outcomes, and a more efficient healthcare system overall. But what does this mean for patients and healthcare providers alike? Well, for starters, it means that healthcare professionals can focus more on what truly matters—providing quality care to patients—while AI handles the heavy lifting behind the scenes.
However, the integration of AI into healthcare isn't without its challenges. There are questions about data privacy, the ethics of automated decision-making, and the need for regulatory frameworks that ensure safety while promoting innovation. As we navigate through this exciting yet complex landscape, it’s essential to consider both the benefits and the potential pitfalls of AI in healthcare.
In this article, we will take a closer look at the impact of AI on diagnostics, its role in personalized medicine, and how it accelerates drug discovery. We'll also discuss the challenges that come with implementing AI in healthcare, including regulatory hurdles and interoperability issues. By the end of this journey, you will have a clearer understanding of how AI is not just a tool, but a transformative force that is paving the way for a healthier future.
- What is AI in healthcare? AI in healthcare refers to the use of artificial intelligence technologies to analyze data, improve patient outcomes, and streamline medical processes.
- How does AI improve diagnostics? AI enhances diagnostics by analyzing medical images and patient data to identify diseases more accurately and quickly.
- What are the ethical concerns surrounding AI in healthcare? Ethical concerns include accountability for decisions made by AI systems, potential biases in algorithms, and the implications of automated decision-making.
- Can AI personalize medicine? Yes, AI can analyze genetic information and patient history to create customized treatment plans that improve outcomes and reduce side effects.
- What challenges does AI face in healthcare? Challenges include resistance to change, high implementation costs, and the need for extensive training among healthcare professionals.

The Impact of AI on Diagnostics
Artificial Intelligence (AI) is not just a buzzword; it is a game-changer in the field of diagnostics. Imagine walking into a doctor's office and having your health concerns addressed with pinpoint accuracy, all thanks to advanced algorithms and machine learning. AI technologies are revolutionizing diagnostic procedures by enhancing both accuracy and speed. This transformation allows healthcare professionals to identify diseases more effectively and tailor treatment plans to individual patients.
For instance, AI can analyze medical images with a level of precision that often surpasses human capabilities. In radiology, algorithms trained on thousands of images can detect anomalies like tumors or fractures that might be overlooked by the human eye. This not only speeds up the diagnostic process but also improves the chances of early detection, which is crucial for conditions like cancer. Furthermore, AI's ability to process vast amounts of data means that it can recognize patterns and correlations that humans might miss, leading to earlier and more accurate diagnoses.
Additionally, AI-driven diagnostic tools can integrate various data sources, including patient history, lab results, and even genetic information. This comprehensive approach enables healthcare providers to gain a holistic view of a patient's health, which is vital for effective treatment planning. For example, a patient presenting with vague symptoms could be quickly assessed through AI algorithms that sift through their medical history and current symptoms, providing a list of potential conditions and suggesting further tests.
However, the integration of AI in diagnostics is not without its challenges. One major concern is the data privacy of patients. As AI systems require access to sensitive health information, safeguarding this data becomes paramount. Healthcare providers must ensure that they comply with regulations such as HIPAA in the United States, which governs patient privacy and data security. Moreover, there is a pressing need for robust ethical guidelines to govern the use of AI in healthcare, ensuring that these technologies enhance rather than hinder patient care.
In conclusion, the impact of AI on diagnostics is profound and multifaceted. By improving accuracy, speeding up processes, and offering personalized insights, AI is paving the way for a new era in healthcare. As we continue to embrace these technologies, it is essential to address the accompanying challenges to fully realize their potential in improving patient outcomes.
- How does AI improve diagnostic accuracy? AI algorithms analyze vast datasets to identify patterns that can lead to more accurate diagnoses.
- What are the risks associated with AI in diagnostics? Risks include data privacy concerns and the potential for algorithmic bias, which can affect patient care.
- Can AI replace human doctors in diagnostics? While AI can enhance diagnostic processes, it is intended to assist healthcare professionals, not replace them.
- How is patient data kept secure when using AI? Healthcare providers must adhere to strict regulations and implement robust security measures to protect patient data.

AI in Personalized Medicine
In today's rapidly evolving healthcare landscape, personalized medicine is emerging as a game-changer, and at the heart of this transformation lies artificial intelligence. Imagine a world where medical treatments are tailored specifically to your unique genetic makeup and health history. This is no longer a distant dream; it's becoming a reality thanks to the innovative capabilities of AI. By analyzing vast amounts of data, AI can help healthcare providers make more informed decisions, leading to better patient outcomes and a reduction in adverse side effects.
One of the most exciting aspects of AI in personalized medicine is its ability to leverage machine learning algorithms. These algorithms can sift through enormous datasets, identifying patterns and correlations that would be impossible for human analysts to detect. For instance, AI can analyze genomic data alongside clinical records to pinpoint the most effective treatment options for individual patients. This means that instead of a one-size-fits-all approach, treatments can be customized to fit the specific needs of each patient, making healthcare more effective and efficient.
However, the integration of AI into personalized medicine is not without its challenges. Data privacy concerns are at the forefront of this discussion. As AI systems process sensitive health information, questions arise about how to protect patient data. Healthcare providers must implement robust security measures to ensure that personal information remains confidential while still harnessing the power of AI. This is crucial because any breach of trust can lead to hesitancy among patients regarding the use of AI in their healthcare.
Moreover, ethical considerations cannot be overlooked. The use of AI raises important questions about accountability and bias. For example, if an AI system makes a recommendation that leads to a negative outcome, who is responsible? Is it the healthcare provider, the software developer, or the institution? Additionally, if the data used to train these AI systems contains biases, there’s a risk that the recommendations will perpetuate those biases, leading to unequal treatment across different demographic groups.
Despite these challenges, the potential benefits of AI in personalized medicine are immense. As healthcare continues to embrace technological advancements, the focus will increasingly shift towards creating a more patient-centered approach. For instance, consider the following potential advantages:
- Improved Treatment Efficacy: Tailored therapies can lead to higher success rates.
- Reduced Side Effects: Personalized treatments can minimize adverse reactions.
- Enhanced Patient Engagement: Patients are more likely to adhere to treatment plans that feel relevant to their personal health needs.
In summary, the intersection of AI and personalized medicine is paving the way for a new era in healthcare. By harnessing the power of advanced algorithms and data analysis, healthcare providers can offer customized treatments that not only improve patient outcomes but also enhance the overall patient experience. As we move forward, it’s essential to address the challenges associated with data privacy and ethical considerations to fully realize the potential of AI in transforming personalized medicine.
- What is personalized medicine? Personalized medicine refers to tailoring medical treatment to the individual characteristics of each patient, often using genetic information.
- How does AI improve personalized medicine? AI analyzes large datasets to identify patterns and correlations that help healthcare providers create customized treatment plans.
- What are the risks associated with AI in healthcare? The main risks include data privacy concerns, ethical dilemmas regarding accountability, and potential biases in AI algorithms.

Machine Learning Algorithms
When we talk about personalized medicine, the term "machine learning algorithms" often pops up, and for good reason! These algorithms are like the detectives of the healthcare world, sifting through mountains of data to uncover hidden patterns that can lead to better treatment options. Imagine having a super-smart assistant who can analyze thousands of patient records, genetic information, and clinical studies in the blink of an eye. That’s what machine learning does! It allows healthcare providers to tailor treatment plans based on individual patient needs, which is a game-changer in improving health outcomes.
But how exactly do these algorithms work? At their core, they are designed to learn from data. They start with a large dataset, which can include everything from medical histories to lab results. As they process this information, they identify trends and correlations that may not be immediately obvious to human practitioners. For example, a machine learning algorithm might discover that certain genetic markers are associated with a higher risk of developing a specific disease. This insight allows doctors to screen patients more effectively and implement preventative measures.
One of the most exciting aspects of machine learning in healthcare is its ability to improve over time. As more data becomes available, these algorithms can refine their predictions and recommendations, leading to increasingly accurate and personalized care. In fact, studies have shown that machine learning models can outperform traditional statistical methods in predicting patient outcomes. This is particularly important in areas like oncology, where understanding the nuances of a patient’s condition can significantly influence treatment decisions.
However, it's essential to recognize that the use of machine learning algorithms in healthcare isn't without challenges. For instance, the quality of the data used is crucial. If the data is biased or incomplete, the algorithms may produce misleading results. Additionally, there are ethical considerations surrounding transparency and accountability. How do we ensure that these algorithms are fair and do not perpetuate existing biases in healthcare? These questions are vital as we move forward with integrating machine learning into medical practices.
To summarize, machine learning algorithms are revolutionizing the way healthcare is delivered. They offer the promise of more personalized, efficient, and effective treatment options. As we continue to develop and refine these technologies, it’s crucial to address the challenges they present, ensuring that they benefit all patients equally. The future of healthcare may very well depend on how well we can harness the power of machine learning while navigating its complexities.
- What are machine learning algorithms? - Machine learning algorithms are computational methods that analyze data to learn patterns and make predictions without being explicitly programmed for specific tasks.
- How do machine learning algorithms improve healthcare? - They enhance healthcare by providing personalized treatment options, predicting patient outcomes, and identifying trends within large datasets.
- What are the challenges associated with machine learning in healthcare? - Challenges include data quality issues, ethical concerns, and the need for transparency in algorithmic decision-making.
- Can machine learning replace healthcare professionals? - No, machine learning is designed to assist healthcare professionals, not replace them. It enhances their ability to make informed decisions.

Data Privacy Concerns
As we dive deeper into the realm of AI in healthcare, one of the most pressing issues that emerge is data privacy. With AI systems processing vast amounts of sensitive health information, the potential for breaches and misuse of data becomes a significant concern. Imagine your personal health records being exposed or used without your consent; it’s a nightmare scenario that many fear could become a reality. The healthcare sector must navigate these turbulent waters carefully to protect patient privacy while still leveraging the incredible capabilities of AI.
To put things into perspective, consider the sheer volume of data generated in healthcare. From electronic health records (EHRs) to genetic information, the data landscape is not only vast but also incredibly personal. This raises several questions:
- How can we ensure that patient data remains confidential?
- What measures are in place to prevent unauthorized access?
- Are healthcare providers fully aware of their responsibilities regarding data protection?
Moreover, the integration of AI introduces additional layers of complexity. For instance, algorithms may inadvertently expose sensitive information through patterns they identify in the data. This phenomenon raises ethical dilemmas regarding informed consent and the extent to which patients understand how their data is being utilized. It’s crucial for healthcare organizations to not only implement robust security measures but also to foster transparent communication with patients about how their data is handled.
In response to these concerns, regulatory bodies are stepping up to establish guidelines that govern the use of AI in healthcare. These regulations aim to ensure that data privacy is prioritized while still allowing for innovation. However, the challenge lies in balancing the need for progress with the necessity of protecting patient rights. For example, the General Data Protection Regulation (GDPR) in Europe sets a high standard for data protection, influencing how AI systems are developed and deployed.
Ultimately, the conversation around data privacy in AI healthcare is ongoing, and it’s essential for all stakeholders—healthcare providers, technology developers, and patients—to engage actively in shaping a future where privacy and innovation coexist. By doing so, we can harness the power of AI while safeguarding the very essence of what makes healthcare personal.
- What is the biggest risk to data privacy in AI healthcare? The biggest risk comes from unauthorized access to sensitive patient data, which can lead to identity theft and misuse of personal information.
- How can patients protect their data? Patients can protect their data by being aware of their rights, understanding how their data is used, and choosing healthcare providers who prioritize data security.
- Are there regulations in place for AI data privacy? Yes, regulations like GDPR in Europe and HIPAA in the United States set standards for data protection in healthcare, including the use of AI technologies.

Ethical Considerations
As we dive deeper into the world of artificial intelligence (AI) within healthcare, it becomes increasingly clear that ethical considerations are paramount. The rapid integration of AI technologies raises critical questions about accountability and bias. For instance, who is responsible when an AI system makes an erroneous diagnosis? Is it the healthcare provider who relied on the AI, the developers of the algorithm, or the institution that implemented it? These questions highlight the need for clear guidelines and accountability frameworks to ensure patient safety and trust.
Moreover, bias in AI algorithms is a significant concern. If the data used to train these systems is skewed or unrepresentative, the outcomes can be detrimental, particularly for marginalized groups. For example, if an AI diagnostic tool is primarily trained on data from a specific demographic, it may not perform accurately for patients outside that group. This can lead to disparities in healthcare delivery, where certain populations receive subpar care due to systemic biases embedded in the technology.
Another ethical dilemma arises from the implications of automated decision-making in critical health scenarios. While AI can process vast amounts of data and provide insights faster than human practitioners, the lack of human intuition and empathy in these decisions can be troubling. Imagine a scenario where an AI system recommends a treatment plan that, while statistically sound, overlooks the patient's personal circumstances and emotional needs. This brings us to the heart of the matter: healthcare is not just about data; it’s about people.
To address these ethical challenges, it is essential to establish a framework that prioritizes:
- Transparency: AI systems should be designed to provide clear explanations for their recommendations, allowing healthcare providers and patients to understand the rationale behind decisions.
- Accountability: Clear lines of responsibility must be established to ensure that all parties involved in the use of AI are held accountable for its outcomes.
- Equity: Efforts must be made to eliminate biases in AI training datasets to ensure fair treatment across diverse populations.
- Human Oversight: AI should augment human decision-making rather than replace it, ensuring that healthcare professionals remain at the forefront of patient care.
In conclusion, while AI holds immense potential to revolutionize healthcare, it is vital to navigate these ethical considerations thoughtfully. By prioritizing transparency, accountability, equity, and human oversight, we can harness the power of AI to enhance patient care without compromising ethical standards.
What are the major ethical concerns regarding AI in healthcare?
The major ethical concerns include accountability for AI decisions, bias in algorithms, and the implications of automated decision-making on patient care.
How can bias in AI algorithms be mitigated?
Bias can be mitigated by using diverse and representative datasets for training AI systems, along with continuous monitoring and evaluation of AI performance across different demographics.
Why is human oversight important in AI healthcare applications?
Human oversight is crucial because AI lacks the ability to understand the emotional and contextual nuances of patient care, which are essential for making informed and compassionate healthcare decisions.

AI in Predictive Analytics
In today's fast-paced healthcare environment, predictive analytics powered by artificial intelligence (AI) is becoming a game-changer. Imagine a world where hospitals can anticipate patient needs before they even arise—this is not science fiction; it is the reality that AI is helping to create. By leveraging vast amounts of data, AI can identify trends and patterns that humans might miss, allowing healthcare systems to react swiftly and efficiently. For instance, AI algorithms can analyze historical patient data, social determinants of health, and even environmental factors to predict potential disease outbreaks. This capability not only enhances patient care but also optimizes resource allocation, ensuring that healthcare providers are prepared for what lies ahead.
One of the most significant advantages of AI in predictive analytics is its ability to improve public health responses. By forecasting disease trends, healthcare organizations can mobilize resources more effectively. For example, during flu season, predictive analytics can help hospitals anticipate surges in patient visits, enabling them to staff appropriately and manage supplies. This proactive approach can significantly reduce wait times and improve patient outcomes. Additionally, AI can aid in identifying high-risk populations, allowing for targeted interventions that can prevent diseases before they escalate.
However, the implementation of AI in predictive analytics is not without its challenges. Data quality and availability are crucial factors that can significantly impact the effectiveness of AI models. In many cases, healthcare organizations struggle with fragmented data systems, making it difficult to gather comprehensive datasets for analysis. Furthermore, AI models are only as good as the data they are trained on, which raises questions about data bias. If the data used to train these models is not representative of the entire population, the predictions made can be skewed, potentially leading to inequitable healthcare outcomes.
To address these challenges, it is essential for healthcare organizations to invest in robust data management systems and ensure that their data is diverse and comprehensive. Collaboration among various stakeholders, including healthcare providers, tech companies, and regulatory bodies, is vital in creating a standardized approach to data sharing and integration. By fostering a culture of collaboration, the healthcare sector can unlock the full potential of AI in predictive analytics, ultimately leading to better patient care and health outcomes.
| Key Benefits of AI in Predictive Analytics | Challenges |
|---|---|
| Improved patient care through proactive interventions | Data quality and availability issues |
| Efficient resource allocation during peak times | Potential data bias affecting predictions |
| Enhanced public health responses to disease outbreaks | Fragmented data systems hindering analysis |
As we look to the future, the role of AI in predictive analytics will undoubtedly continue to expand. With the right investments in technology and training, healthcare providers can harness the power of AI to not only predict health trends but also to revolutionize the way they deliver care. The integration of AI tools into everyday practices will pave the way for a more responsive, efficient, and effective healthcare system that ultimately prioritizes patient well-being.
- What is predictive analytics in healthcare?
Predictive analytics in healthcare refers to the use of statistical algorithms and machine learning techniques to identify the likelihood of future outcomes based on historical data. This can help in anticipating patient needs and improving healthcare delivery. - How does AI enhance predictive analytics?
AI enhances predictive analytics by processing large datasets quickly and accurately, identifying patterns and trends that can inform healthcare decisions and resource allocation. - What are the challenges of implementing AI in predictive analytics?
Some challenges include data quality and availability, potential bias in data, and the need for collaboration among various healthcare stakeholders to ensure effective integration.

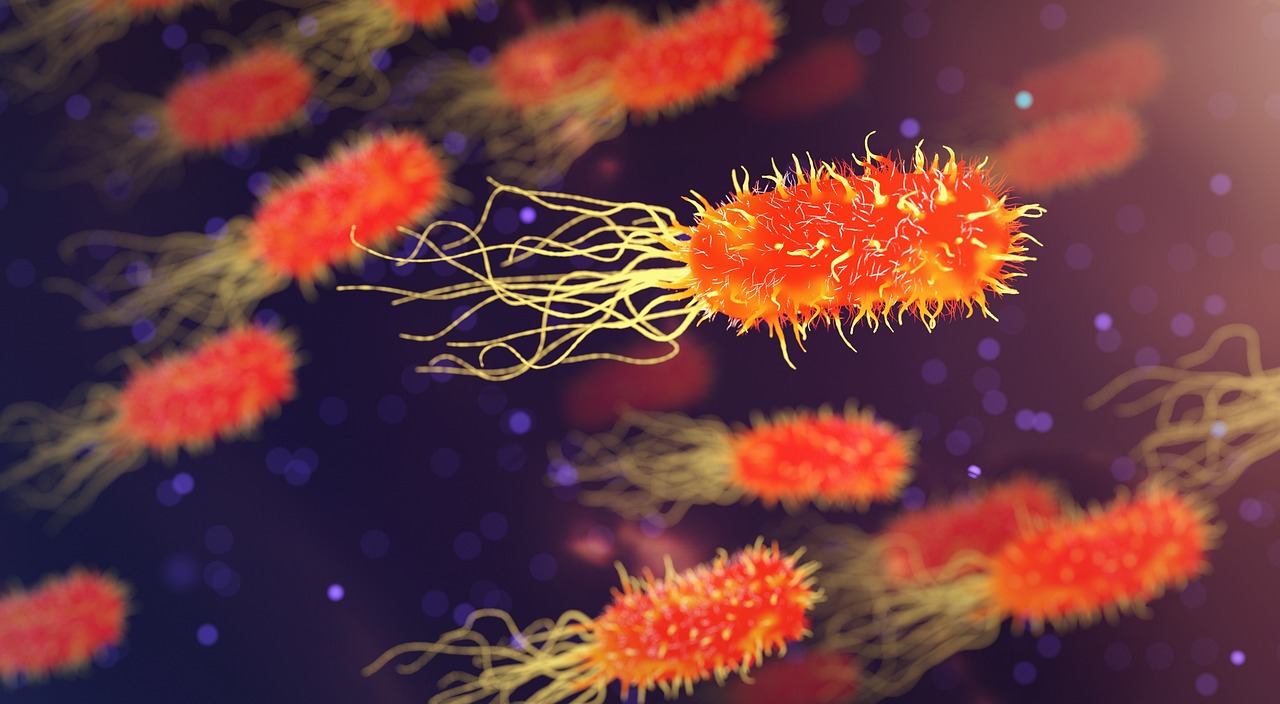
AI's Role in Drug Discovery
The landscape of drug discovery is undergoing a remarkable transformation, thanks to the integration of artificial intelligence (AI). This innovative technology is not just a buzzword; it’s a game-changer that accelerates the process of discovering new medications. Traditionally, drug discovery has been a lengthy and costly endeavor, often taking over a decade and billions of dollars to bring a new drug to market. However, with AI stepping into the spotlight, the timeline is shrinking, and the costs are plummeting.
At its core, AI enhances the ability to analyze molecular data, which is crucial in identifying potential drug candidates. By leveraging vast datasets, AI algorithms can sift through complex biological information at lightning speed, uncovering patterns and relationships that might elude even the most experienced researchers. This capability not only expedites the identification of viable drug candidates but also allows for a more targeted approach, ensuring that the right compounds are prioritized for further development.
One of the most exciting aspects of AI in drug discovery is its ability to predict how different molecules will interact with biological targets. This predictive power can significantly reduce the number of compounds that need to be tested in the lab, saving both time and resources. Imagine a scenario where researchers can simulate the effects of a drug on a virtual model of the human body before any actual testing occurs. This not only enhances efficiency but also minimizes the risks associated with drug development.
Furthermore, AI can streamline the entire process of clinical trials. By analyzing patient data, AI can help identify suitable participants for trials, ensuring that the right demographics are represented. This targeted recruitment is crucial for the success of clinical trials as it increases the likelihood of favorable outcomes and reduces the time needed to gather sufficient data. AI can also predict trial outcomes based on historical data, allowing researchers to refine their approaches and increase the chances of success.
To illustrate the impact of AI on drug discovery, consider the following table showcasing the traditional drug discovery timeline compared to the AI-enhanced approach:
| Phase | Traditional Timeline | AI-Enhanced Timeline |
|---|---|---|
| Target Identification | 1-2 years | Weeks to months |
| Lead Compound Discovery | 2-4 years | Months |
| Preclinical Testing | 1-2 years | Months |
| Clinical Trials | 6-10 years | 3-5 years |
| Total Time to Market | 10-15 years | 4-7 years |
As we can see, AI not only compresses the timeline but also enhances the overall efficiency of the drug discovery process. However, it’s important to note that while AI is making significant strides, it is not without its challenges. Issues such as data quality, regulatory hurdles, and the need for interdisciplinary collaboration must be addressed to fully harness the potential of AI in this field.
In conclusion, the role of AI in drug discovery is a beacon of hope for the future of medicine. By accelerating the identification and development of new drugs, AI is set to revolutionize the pharmaceutical industry, ultimately improving patient outcomes and making healthcare more accessible. As we continue to explore the possibilities of AI, one thing is clear: the future of drug discovery is bright, and the innovations are just beginning.
- What is the primary benefit of using AI in drug discovery? AI significantly reduces the time and cost associated with bringing new drugs to market by enhancing data analysis and predictive capabilities.
- How does AI improve clinical trials? AI streamlines participant recruitment and predicts trial outcomes, increasing the efficiency and success rates of clinical evaluations.
- Are there any challenges associated with AI in drug discovery? Yes, challenges include data quality, regulatory hurdles, and the need for collaboration among various stakeholders.

Accelerating Clinical Trials
In the realm of healthcare, clinical trials are the backbone of medical advancement, serving as the critical testing ground for new therapies and treatments. However, traditional clinical trial processes can often be slow, cumbersome, and fraught with inefficiencies. Enter artificial intelligence (AI) — a game changer that is revolutionizing how we conduct clinical trials. By harnessing the power of AI, researchers can dramatically accelerate the entire process, from participant recruitment to data analysis.
One of the most significant advantages of AI in clinical trials is its ability to identify suitable participants more efficiently. Traditionally, finding the right candidates for a trial can take months, if not years. AI algorithms can sift through vast databases of patient records, genetic information, and health histories to pinpoint individuals who meet specific criteria. This not only speeds up recruitment but also enhances the likelihood of successful outcomes by ensuring that the right patients are included in the study.
Moreover, AI can assist in predicting outcomes based on historical data. By analyzing previous trial results and patient responses, machine learning models can offer insights into which treatments are likely to be more effective for certain demographics or conditions. This predictive capability allows researchers to refine their trial designs, focusing on more promising avenues and potentially saving millions in development costs.
| Benefits of AI in Clinical Trials | Description |
|---|---|
| Faster Recruitment | AI streamlines the process of identifying eligible participants, reducing the time needed to fill trial cohorts. |
| Enhanced Data Analysis | AI algorithms can analyze complex datasets quickly, providing insights that inform trial adjustments and strategies. |
| Cost Efficiency | By optimizing processes and reducing trial duration, AI can significantly lower the overall costs associated with drug development. |
Another area where AI shines is in the monitoring of trials. Once a clinical trial is underway, AI can continuously analyze data in real-time, identifying any adverse effects or trends that may arise. This capability allows for swift action, ensuring participant safety and maintaining the integrity of the trial. Additionally, AI can facilitate adaptive trial designs, where protocols can be adjusted based on interim results, further enhancing the efficiency of the process.
However, while the benefits of AI in accelerating clinical trials are substantial, there are still challenges to address. Issues such as data privacy, regulatory compliance, and the need for robust AI infrastructure must be navigated carefully. As we move forward, it is crucial for stakeholders in the healthcare sector to collaborate and create standards that ensure the ethical and effective use of AI in clinical research.
- What role does AI play in participant recruitment for clinical trials?
AI helps identify and recruit suitable participants by analyzing large datasets to match individuals with specific trial criteria, thereby speeding up the recruitment process. - Can AI improve the accuracy of clinical trial outcomes?
Yes, AI can analyze historical data to predict outcomes, allowing researchers to refine trial designs and focus on more promising treatments. - What are the risks associated with using AI in clinical trials?
Risks include data privacy concerns, the need for regulatory compliance, and potential biases in AI algorithms that could affect trial results.

Collaborative Robots in Surgery
The rise of collaborative robots, often referred to as cobots, in the surgical field is nothing short of revolutionary. These advanced machines are designed to work alongside human surgeons, enhancing their capabilities and transforming the surgical landscape. Imagine a scenario where a surgeon, equipped with a high-tech robotic assistant, can perform intricate procedures with unparalleled precision. This is not science fiction; it's the reality of modern medicine. Cobots are engineered to assist in various surgical tasks, from suturing to complex organ manipulation, thereby minimizing human error and improving patient outcomes.
One of the most compelling advantages of using collaborative robots in surgery is their ability to reduce recovery times. Traditional surgical methods often require large incisions, leading to longer healing periods and increased risk of complications. In contrast, cobots enable minimally invasive techniques, allowing for smaller incisions and less trauma to the body. This not only shortens hospital stays but also enhances the overall patient experience. Patients can return to their daily lives much quicker, which is a significant benefit in today’s fast-paced world.
Furthermore, the integration of cobots in surgical procedures allows for greater consistency and repeatability. These robots can perform tasks with a level of accuracy that is difficult for even the most skilled human hands to achieve. For instance, in delicate procedures such as neurosurgery or orthopedic operations, the precision of a robot can make a world of difference. By ensuring that movements are exact and measured, cobots help in reducing the likelihood of complications during and after surgery.
However, it's essential to recognize that the introduction of collaborative robots in surgery does not aim to replace human surgeons. Instead, it enhances their capabilities and allows them to focus on more critical aspects of patient care. The synergy between human intelligence and robotic precision creates a powerful combination that can lead to better surgical outcomes. Surgeons can leverage the strengths of cobots to make informed decisions during procedures, ultimately leading to improved patient safety and satisfaction.
Despite the numerous benefits, the adoption of collaborative robots in surgery does come with its own set of challenges. Training healthcare professionals to work effectively with these machines is crucial. Surgeons must not only understand how to operate the robots but also how to interpret the data and insights generated by them. Additionally, the cost of implementing such advanced technology can be a barrier for many healthcare institutions, particularly smaller facilities. As the technology continues to evolve and become more accessible, we can expect to see a broader implementation of cobots across various surgical specialties.
In conclusion, collaborative robots are paving the way for a new era in surgery, characterized by enhanced precision, reduced recovery times, and improved patient outcomes. As we continue to explore the potential of these innovative machines, the future of surgery looks promising. The blend of human skill and robotic assistance is not just a trend; it’s a significant leap toward a more efficient and effective healthcare system.
- What are collaborative robots? Collaborative robots, or cobots, are robotic systems designed to assist human surgeons during surgical procedures, enhancing precision and efficiency.
- How do cobots improve surgical outcomes? Cobots reduce human error, allow for minimally invasive techniques, and provide consistent, precise movements, leading to better patient outcomes.
- Are cobots replacing human surgeons? No, cobots are designed to assist and enhance the capabilities of human surgeons, not replace them.
- What challenges are associated with using cobots in surgery? Challenges include the need for extensive training for healthcare professionals and the high costs of implementing this technology in healthcare settings.

Challenges of Implementing AI in Healthcare
The journey of integrating artificial intelligence into healthcare is not without its hurdles. While the potential benefits of AI are immense, the road to successful implementation is often paved with challenges that can deter even the most enthusiastic healthcare providers. One of the primary challenges is the resistance to change. Many healthcare professionals are accustomed to traditional methods and may be hesitant to embrace new technologies that require a shift in their workflow. This resistance can stem from a lack of understanding of AI's capabilities and benefits, leading to skepticism about its effectiveness in improving patient care.
Additionally, the financial implications of adopting AI technologies can be daunting. The costs associated with acquiring AI systems, training staff, and maintaining the technology can be significant, particularly for smaller healthcare facilities. This financial burden can create a barrier to entry, limiting access to advanced tools that could enhance patient outcomes. Furthermore, the complexity of AI systems often necessitates extensive training for healthcare professionals, which can be time-consuming and resource-intensive.
Another critical aspect to consider is the regulatory hurdles that AI technologies face. Navigating the intricate landscape of healthcare regulations is essential for ensuring that AI solutions are safe and effective. Regulatory bodies must establish clear guidelines for the approval and deployment of AI technologies, which can be a slow and cumbersome process. This delay in regulatory approval can hinder innovation and slow down the adoption of potentially life-saving technologies.
Moreover, interoperability issues present another significant challenge. For AI systems to function effectively within the healthcare ecosystem, they must be able to communicate seamlessly with existing technologies. This requires a standardized approach to data sharing and collaboration among various stakeholders, including healthcare providers, technology developers, and regulatory agencies. Without interoperability, the full potential of AI cannot be realized, leading to fragmented care and inefficient workflows.
In summary, while the integration of AI into healthcare holds great promise, it is crucial to address the challenges that accompany this transformation. By fostering a culture of openness to change, investing in training, navigating regulatory landscapes, and ensuring interoperability, the healthcare sector can harness the power of AI to improve patient care and outcomes.
- What are the main challenges of implementing AI in healthcare?
Resistance to change, high costs, regulatory hurdles, and interoperability issues are among the significant challenges faced. - How can healthcare professionals overcome resistance to AI?
Education and training about AI's benefits can help alleviate skepticism and encourage adoption. - Why is regulatory approval important for AI technologies?
Regulatory approval ensures that AI systems are safe and effective for patient care, fostering trust among healthcare providers. - What does interoperability mean in the context of AI?
Interoperability refers to the ability of AI systems to work seamlessly with existing healthcare technologies, allowing for efficient data sharing and communication.
Regulatory Hurdles
As the integration of artificial intelligence (AI) into healthcare accelerates, navigating the regulatory landscape becomes increasingly complex. Regulatory hurdles are a significant barrier to the widespread adoption of AI technologies in medical settings. These hurdles stem from the need to ensure patient safety and the efficacy of AI systems before they can be deployed in clinical environments.
One of the primary challenges is the lack of standardized regulations that specifically address AI applications in healthcare. While traditional medical devices and drugs have well-established approval processes, AI systems often fall into a gray area. Regulatory bodies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), are still developing frameworks for evaluating AI technologies. This can lead to delays in bringing innovative solutions to market, ultimately hindering patient access to potentially life-saving treatments.
Moreover, the dynamic nature of AI algorithms poses another challenge. Unlike static medical devices, AI systems can evolve and improve over time through machine learning. This raises questions about how often these algorithms should be re-evaluated and whether they require new approvals as they adapt. Regulatory bodies must find a balance between ensuring safety and innovation, which is no easy feat.
To illustrate the regulatory challenges faced by AI in healthcare, consider the following table:
| Challenge | Description | Potential Solutions |
|---|---|---|
| Lack of Standardization | Absence of uniform regulations for AI applications in healthcare. | Development of comprehensive guidelines by regulatory bodies. |
| Dynamic Algorithms | AI systems that evolve may require ongoing evaluations. | Creating adaptive regulatory frameworks that account for algorithm updates. |
| Data Privacy Issues | Ensuring patient data security while using AI technologies. | Implementing strict data protection regulations and compliance measures. |
Furthermore, the collaboration between regulatory agencies and AI developers is crucial. Engaging in dialogue can help regulators understand the technology better, leading to more informed decision-making. This partnership can also foster a culture of transparency, where developers are encouraged to share data and outcomes from their AI systems, thus enhancing trust in these technologies.
In conclusion, while regulatory hurdles present significant challenges to the implementation of AI in healthcare, they are not insurmountable. With proactive measures, collaboration, and a commitment to patient safety, the healthcare industry can navigate these obstacles and unlock the full potential of AI technologies.
- What are the main regulatory bodies overseeing AI in healthcare? The primary regulatory bodies include the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA).
- Why is standardization important for AI in healthcare? Standardization ensures consistent safety and efficacy evaluations, facilitating faster and more reliable approvals for AI technologies.
- How can AI developers help with regulatory challenges? By engaging with regulatory bodies and sharing data transparently, AI developers can contribute to the development of effective regulations.

Interoperability Issues
When it comes to the integration of artificial intelligence in healthcare, one of the most significant challenges that arises is interoperability. This term refers to the ability of different systems, devices, and applications to communicate and exchange data effectively. In a world where healthcare is becoming increasingly digitized, ensuring that AI systems can seamlessly interact with existing healthcare technologies is essential. Imagine trying to send a text message from one phone brand to another but finding that the two systems can't talk to each other; that's essentially what interoperability issues can feel like in the healthcare landscape.
In order to achieve true interoperability, several factors come into play. First and foremost is the need for standardization. Without common standards, data formats, and protocols, the potential of AI in healthcare remains limited. For instance, if one hospital uses a specific AI tool that analyzes patient data in a certain format, but another hospital employs a different system that doesn't recognize that format, the valuable insights derived from AI could be lost in translation. This not only hampers the clinical decision-making process but can also lead to delays in patient care.
Moreover, collaboration among various stakeholders in the healthcare ecosystem is vital. This includes healthcare providers, technology developers, and regulatory bodies. Each of these entities has its own set of priorities and requirements, which can complicate efforts to create a cohesive system. For example, while healthcare providers may prioritize patient care and outcomes, technology developers might focus on innovation and functionality. Finding common ground is crucial for overcoming interoperability challenges.
Another layer of complexity is added by the sheer volume of data generated in healthcare settings. With the rise of electronic health records (EHRs), wearable devices, and telemedicine, the amount of data available for analysis is staggering. AI systems need to be capable of processing this data from multiple sources in real-time, which requires robust infrastructure and advanced algorithms. Without these capabilities, the promise of AI to improve patient outcomes and streamline healthcare processes remains unfulfilled.
To illustrate the importance of interoperability, consider a scenario where a patient visits multiple specialists for different health issues. If each specialist uses a separate AI tool that cannot share data with the others, critical information may be overlooked, leading to misdiagnosis or inappropriate treatment. Therefore, fostering interoperability is not just a technical challenge; it is a matter of patient safety and quality of care.
In conclusion, addressing interoperability issues in AI healthcare integration is essential for maximizing the benefits of these technologies. By focusing on standardization, collaboration, and infrastructure development, the healthcare industry can pave the way for a more connected and efficient future. The road may be challenging, but the potential rewards in terms of improved patient outcomes and streamlined processes are worth the effort.
- What is interoperability in healthcare? Interoperability in healthcare refers to the ability of different systems and applications to communicate and exchange data effectively.
- Why is interoperability important for AI in healthcare? Interoperability is crucial for AI in healthcare as it ensures that different systems can work together, facilitating better patient care and more efficient processes.
- What are the challenges of achieving interoperability? Challenges include the need for standardization, collaboration among stakeholders, and the ability to process large volumes of data from various sources.
- How can interoperability be improved? Interoperability can be improved through the establishment of common standards, better communication among healthcare providers and technology developers, and investment in robust infrastructure.
Frequently Asked Questions
- What are the main benefits of AI in healthcare?
AI enhances diagnostic accuracy and speed, personalizes treatment plans, and improves patient outcomes. By analyzing vast amounts of data, AI can identify patterns that help healthcare professionals make informed decisions, ultimately leading to better care.
- How does AI improve diagnostics?
AI technologies, such as machine learning algorithms, analyze medical images and patient data to detect diseases more effectively. This allows for quicker diagnoses, enabling healthcare providers to start treatment sooner and tailor it to individual needs.
- What is personalized medicine, and how does AI contribute to it?
Personalized medicine involves customizing healthcare based on individual patient characteristics. AI plays a crucial role by analyzing genetic information and medical history, allowing for tailored treatment plans that enhance effectiveness and minimize side effects.
- Are there privacy concerns with AI in healthcare?
Yes, as AI systems handle sensitive health data, there are significant concerns regarding patient privacy and data security. It's essential for healthcare organizations to implement robust measures to protect personal information while leveraging AI's capabilities.
- What ethical issues arise from using AI in healthcare?
The use of AI raises questions about accountability, potential biases in algorithms, and the implications of automated decision-making, particularly in critical health scenarios. Addressing these ethical considerations is vital for responsible AI implementation.
- How does AI assist in drug discovery?
AI accelerates drug discovery by analyzing molecular data and identifying promising candidates for new medications. This significantly reduces the time and costs associated with bringing new drugs to market, making the process more efficient.
- What challenges does AI face in healthcare implementation?
Challenges include resistance to change among healthcare professionals, high costs of AI technologies, and the need for extensive training. Overcoming these hurdles is essential for the successful integration of AI in healthcare systems.
- What are regulatory hurdles for AI in healthcare?
Navigating regulatory frameworks is crucial for the safe deployment of AI technologies. Ensuring compliance with safety and efficacy standards while fostering innovation is a balancing act that healthcare organizations must manage.
- How important is interoperability for AI systems in healthcare?
Interoperability is essential for seamless integration of AI systems with existing healthcare technologies. Standardization and collaboration among stakeholders are necessary to ensure that AI can effectively communicate and operate within the healthcare ecosystem.